by Bag It Team | Aug 11, 2021 | Educational Articles
 August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
Did you know…
- About 25% of cancer deaths are from lung cancer – that’s more than colon, breast and prostate cancer deaths combined. (But the good news is that fewer Americans are smoking these days and new lung cancer treatments have been very effective in controlling some types of advanced disease.)
- Active cigarette smoking is by far the leading cause (about 80-90%) of lung cancer, but air pollution, secondhand smoke and other chemicals in the home and workplace, and family history, are also risk factors.
- While some experience symptoms related to the lungs, most people with lung cancer don’t have symptoms until the cancer is advanced.
- If you are at high risk*, an annual low-dose CT scan to screen for lung cancer may save your life. It can detect lung cancer earlier, when it is more treatable. Speak with your doctor about your personal health history and screening risks, as it is not recommended for everyone.

*(i.e. 1 pack a day for 20 years, 2 packs a day for 10 years, etc.)
Click here to order a lung cancer-specific or standard Bag it bag for yourself or as a gift for someone else. (available in English and Spanish)

by Mindy Griffith | Apr 8, 2021 | Educational Articles
Bag It. Guiding one through cancer.
 So, it’s National Read a Roadmap week, and I love a bizarre holiday that connects to many things I love and makes me smile. First, I recall being on a road trip a few years ago, and yes we had GPS on our phones and were using that, when we were trying to find maps of the area we were in just because (okay maybe I wanted to use them later to scrapbook the adventure). At the 3rd gas station we found one, it was dated and covered in dust and the employees thought my friend was crazy for wanting one but we were thrilled!
So, it’s National Read a Roadmap week, and I love a bizarre holiday that connects to many things I love and makes me smile. First, I recall being on a road trip a few years ago, and yes we had GPS on our phones and were using that, when we were trying to find maps of the area we were in just because (okay maybe I wanted to use them later to scrapbook the adventure). At the 3rd gas station we found one, it was dated and covered in dust and the employees thought my friend was crazy for wanting one but we were thrilled!
Then a friend was visiting me and in the side panel of my car I have a few maps, because you never know when you might need one. She found this hilarious and took a picture of it to post on social media asking people if they even knew what they were – she couldn’t believe that I had them in my car. (FYI: I have used them from time to time.)
Now I love technology and frequently use digital maps, but it’s always good to have a back-up plan as we know that technology doesn’t work everywhere or your might not have your phone charged or maybe you just appreciate having things in a printed format. Print makes things easier to share and more readily available (but I encourage you to order those maps in advance of your next trip).
 How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
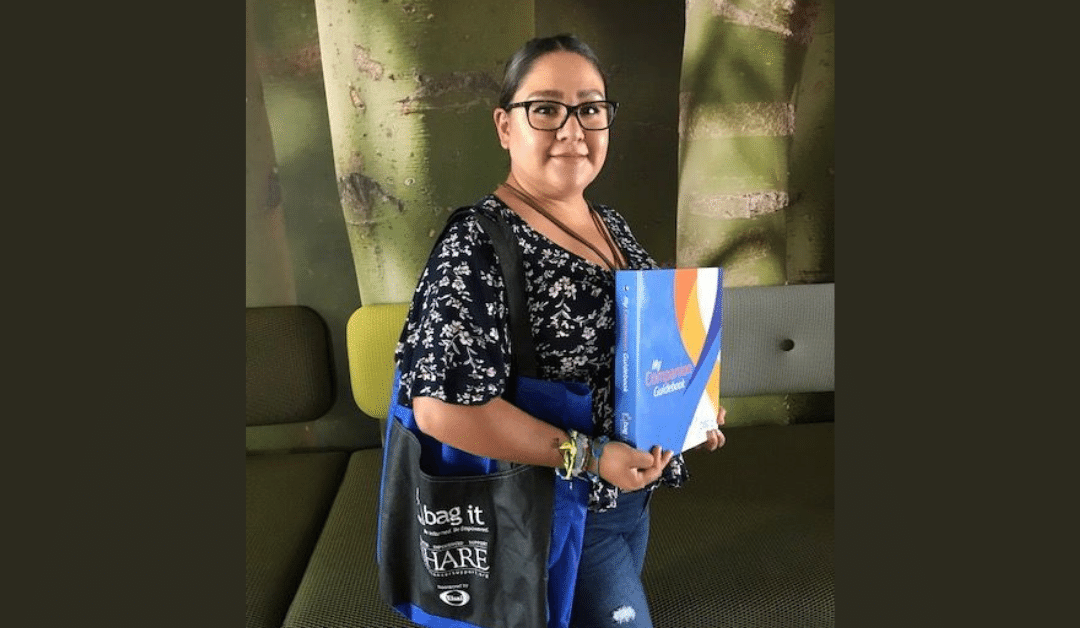
Reading a roadmap takes some practice, just like understanding cancer. The Bag It bag works as a guide to help those impacted by cancer understand more about their diagnosis and cope with the bumps along the way. When you receive a cancer diagnosis you don’t get the map (digital or print) to go with it. You don’t know the vocabulary, the questions to ask, which treatment to take, or which exit has a support network. You need something to help familiarize you with this experience. Your healthcare team is one guide and a Bag It bag is another valuable guide.
The take-everywhere binder (yep, even on that road trip) helps organize appointments and records (similar to your brochures and itineraries). The booklets provide coping tips, support information, reliable cancer information and questions to ask. It’s all in the bag! You won’t feel lost during or after treatment with Bag It as your guide.
Bag It wants to ensure anyone who wants or needs a bag has them available to them. You can order one as a gift for someone when they are diagnosed with cancer to help them cope or you can order/request one for yourself. They are a doctor-recommended resource for anyone with any type of cancer.
If you don’t currently know anyone who could benefit consider participating in our Spring 2021 Fundraiser – Gift a Bag It Bag. With a $41 contribution you can help provide a source of comfort and the printed navigation tools to help a patient throughout their cancer treatment and beyond.

by Mindy Griffith | Feb 3, 2021 | Events

February is a busy month! We honor love, Martin Luther King Jr., Black history, and even our American presidents, but did you know that World Cancer Day also falls in February? The Union for International Cancer Control (UICC) leads the charge in urging everyone to take steps to ensure that preventable cancer deaths are reduced and that there is increased access to life-saving treatments for all patients, “no matter who you are or where you live”. Each year, the UICC establishes a theme for their initiative to shape the many activities and events that kick off around the world each February. This year, the theme is “I Am and I Will” – a call to action to commit and act on steps to get screened and share knowledge in hopes of reducing the number of cancer-related deaths and noncommunicable diseases by one third by 2030 (that’s only 9 years away, so let’s get to it!)

Bag It is aligned with the UICC by providing resources to educate and support patients through their healthcare plan, increasing access to life-saving information regardless of one’s ethnicity or socio-economic background. Bag It provides the tools you need to help you feel more comfortable and confident in speaking up for yourself to ensure the best quality of life with cancer. The contents in the bag are designed to help you and your caregiver(s) cope with the diagnosis, get yourself organized and better understand the language of cancer.
February is cancer prevention month, and we encourage you to think about ways that you can help yourself and others prevent cancer. It’s the perfect time to schedule appointments for you and your loved ones because adhering to the recommended screenings for breast, cervical, colorectal (colon) and lung cancers can lead to early stage diagnosis, which increases the likelihood of treatment working.
What action will you take as we kick off World Cancer Day? Take the 21-Day challenge to learn more about cancer and how to reduce your cancer risks. Some suggestions:
As part of my campaign I participated in the World Cancer Day 21-Day Challenge which was informative and easy and I wrote this blog: I will schedule my mammogram (and a colonoscopy this year) and encourage people to schedule their appointments, and I will work to ensure that everyone diagnosed with cancer receives a Bag It bag to help them cope with their diagnosis and feel comfortable and confident speaking up to ensure they are living their best life with cancer.
Sending positive vibes your way,
Mindy
Preventcancer.org recommends these seven steps to help prevent cancer.

by Mindy Griffith | Jan 6, 2021 | Videos
By Mindy Griffith
“As part of our Wellness Wednesday series Mindy talks about being prepared for appointments in your role of advocating for yourself.
To see more of our Wellness Wednesday videos just click here
by Annettra Farrington | Dec 9, 2020 | Educational Articles
 There is a wide variety of relaxation techniques* out there to try in addition to or to pair with your breathing exercises. Sample a few to find the one that is most helpful to you. Regular practice is the key to continued and more profound benefits.
There is a wide variety of relaxation techniques* out there to try in addition to or to pair with your breathing exercises. Sample a few to find the one that is most helpful to you. Regular practice is the key to continued and more profound benefits.
These are just a few:
- Progressive Muscle Relaxation – this technique involves tightening and then relaxing muscle groups of the body as you take slow, deep breaths, usually while lying down. You can self-guide as you work your way up your body or listen to a recording that will lead you through the exercise.
- Yoga – an ancient practice generally involving your breath and moving through different body poses which may include some meditation. There are many types and levels of yoga that can be enjoyed solo or in a group setting led by a yoga teacher. Classes of all levels can be found in your local community or online. A consistent yoga practice will yield increased benefits. Check with your doctor regarding any health conditions before beginning a new yoga practice.
- Meditation – a mind-body practice to increase your awareness of the present moment and promote calmness and relaxation. There are many different types of meditation which focus one’s attention using the breath, mantra, words or an object. Meditation can be guided (sometimes easier when getting started) or self-directed; it can be short or longer in duration. A consistent daily practice typically becomes easier over time and is highly recommended for maximum benefit.
- Visualization (also known as Guided Imagery) – focus your awareness on a pleasing and calming scenario that can be a place, a memory or sensory elements all of your choosing. You can use a guide or pick an environment of your own making.
Links:
Guided-Imagery Meditation from Memorial Sloan Kettering
Other meditations from Memorial Sloan Kettering Integrative Medicine
Gentle Yoga Poses from Memorial Sloan Kettering Integrative Medicine
Healthline’s best meditation apps for 2020
More relaxation techniques with instructions
*Relaxation techniques are generally considered safe for those who are healthy. People with serious physical or mental health problems should discuss relaxation techniques with their health care providers.
 August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.


 So, it’s
So, it’s  How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?



 There is a wide variety of relaxation techniques* out there to try in addition to or to pair with your breathing exercises. Sample a few to find the one that is most helpful to you. Regular practice is the key to continued and more profound benefits.
There is a wide variety of relaxation techniques* out there to try in addition to or to pair with your breathing exercises. Sample a few to find the one that is most helpful to you. Regular practice is the key to continued and more profound benefits.
Recent Comments