by Bag It Team | Feb 11, 2025 | Educational Articles
February 4th was World Cancer Day. The theme for 2025-2027 is United by Unique.
Each person’s story from diagnosis and beyond is different and each one matters! We receive different diagnoses, advice, treatment plans, drugs, surgeries, care, etc. But cancer is so much more than just a diagnosis.
We go through different emotions and at different paces. We learn so much about ourselves and those we care about. We discover how unique we truly are. Yet in our individuality, comes a kinship. Our story is ours, yet it will resonate with another’s heart.
We are extremely grateful to our Escape to THRIVE participants who were willing to share some of their stories that may touch your heart, may help you find something you’ve been missing, or may just be what you needed to hear to know that you are not alone.
Sharing Cancer Stories
It’s world cancer day today and I am so privileged to still be here while so many of my beautiful friends are not. Today I am so so lucky to be a stage 3C TNBC survivor because there were moments (shit there are still moments) where this crap is so heavy. Being diagnosed young and when you are supposed to be building a family, a home, a future sucks but I’m also thankful, I’m thankful for the compassion and desire to overcome what cancer has taught me. I’m thankful to the doctors and nurses and medicine that saved my life in 2021 so I can be here with no evidence of disease 4 years later. I’m thankful for the perspective cancer has given me not only on life but also death. Most of all I’m thankful for the community cancer helped form for me. A group of other compassionate, powerful, strong, intelligent humans all with this same crappy connection.
—Kimberly
This World Cancer Day I’m choosing to focus on the word grateful. That may seem odd when talking about a cancer diagnosis and, trust me, my heart has not filled with gratitude every day of this journey. I’ve had (and have) many days I look at the changes in my body and I wonder why this happened. But, as difficult as the journey has been at times, it has brought so much to be grateful for into my life.
I am grateful that my cancer was found early. I am grateful that I had an amazing team of doctors who worked together for the best outcomes possible. I am grateful for the family and friends that surrounded me and supported me throughout 7 surgeries and recoveries, especially my saint of a husband. I am grateful for the new friends I have gained in my life from joining a cancer group. And I am grateful for the opportunity I have to give back to those on this journey.
—Amy
This World Cancer Day, I focus on being. In a world full of doing, cancer was a wake up call for me to slow down and just be. Even when I had all the intention in the world to “do” my work continuing education credits during my month long surgery recovery, my body had other plans. I literally could do very little beyond look out the window. Even taking a walk was a momentous event. Slowly, my physical strength came back, and my spiritual and mind space expanded beyond where it had ever been before cancer. Cancer changed my life for the better (I can only say this many years into my thrivership).
I learned to:
- appreciate me for who I am, not the things that I do
- be graceful in accepting help (realizing it is a gift to give, and in order for someone to give help, someone must receive).
- slow down and not do everything everywhere all at once, especially for everyone else
- take time for myself
- advocate for myself and other cancer thrivers
- do the things that I enjoy, including retreats
- meditate
- be even more grateful
- savor each moment, even the challenging ones
- appreciate that growth comes from the seemingly hardest experiences
- heal with nature
Thank you to all of you who have shared in my journey. I am inspired by you. I appreciate you. I am grateful.
—Su-Yen
I see my life in 2 distinct halves: BC and AC—before cancer and after cancer.
I don’t even know that girl BC anymore. It’s as if she once existed and then she…didn’t. Maybe she died all at once while our body was in an icu bed, in a coma, tubes coming from her face, arms tethered, voiceless but wanting to scream, aware but not understanding, asleep but knowing even as she was being drugged into oblivion… Maybe she died little by little, piece by piece, as she lost body parts, left on operating room floors. Maybe she went mad and jumped off a building somewhere. No one noticed she was gone, except me. But I know. I know she’s dead and gone and I cannot deny that the me left in her place is brand new.
AC me has the wisdom that other me never grew old enough to attain. Expansiveness that other me could never begin to comprehend. She is more whole than she was before the mutinous body parts were cut away. She knows love like it’s a way of life. She drinks in experiences like they’re life-giving water. She knows her life purpose like it was tattooed on her soul.
She lives her life as if it is not a promise at all, but a blessing.
—Dawn
I was trained in journalism and beginning in 1984 became attracted to educating patients so they could be more in control of their care. That consumerism was new. In 1996 it became much more personal for me when I was diagnosed with leukemia. Other patients connected me with specialists far from my home and I entered a clinical trial that worked! That survival fueled even more passion to help inform patients and that has propelled me for decades. I feel the reason I survived was for this purpose and it is thrilling to see how better informed patients get better care.
I am 74 years old now and the blood cancer I have, myelofibrosis, is somewhat progressive. But I am NOT slowing down. We patients can help each other and I am delighted to be an active part of the cancer community and help amplify key information that is significant. I believe progress is real and we patients are integral to making it happen!
—Andrew

by Bag It Team | Dec 9, 2024 | Educational Articles
The holiday season can be exhausting for anyone, but cancer-related fatigue is a unique challenge. This type of fatigue goes beyond ordinary tiredness. It’s a deep, persistent fatigue or exhaustion that doesn’t improve with rest or sleep, often leaving you feeling unable to carry out your usual activities.
Cancer-related fatigue is a very common issue and can result from several factors, including:
- The cancer itself or other medical conditions.
- Treatments like chemotherapy, radiation, or surgery, and their side effects.
- Medications you’re taking.
- Changes in blood counts.
- Lifestyle factors, such as sleep disruptions, poor nutrition, or inadequate hydration.
- Emotional or mental health struggles, which fatigue can worsen.
You Don’t Have to Endure It Alone
Share your symptoms with your healthcare team so they can identify possible causes and suggest medical and non-medical treatments to help you.
Let loved ones know how you’re feeling—they often want to help but may not know how. Work together to adjust holiday traditions—whether it’s scaling back on celebrations, delegating or sharing tasks like decorating or cooking, or simplifying shopping. Focus on the activities that matter most to you and bring joy.
And yes, naps are absolutely allowed!
Self-Care Strategies for Cancer-Related Fatigue
These tips can help manage fatigue during the holidays and beyond:
- Set priorities. Choose manageable goals, establish routines, and let go of less important tasks. Don’t hesitate to ask for help.
- Balance activity and rest. While conserving energy is essential, staying physically active—even with gentle movement—can boost energy. Ask your healthcare team about safe exercise options.
- Take breaks. Schedule rest or relaxation time during the day, and don’t wait until you’re overtired.
- Improve sleep quality. Follow a bedtime routine to support better rest at night.
- Eat well and stay hydrated. Aim for a balanced diet. Meeting with a registered dietitian or nutritionist can help you to manage treatment side effects, maintain energy, address weight changes, and create tailored meal plans to support overall health and recovery.
- Care for your emotional health. Spend time with people who uplift you, and communicate your feelings—whether happy, sad, or tired. Alternatively, if you need solitude, it’s okay to set boundaries. You decide what feels right.
- Explore complementary therapies. Discuss with your healthcare provider options like acupuncture, massage, yoga, Tai Chi, Reiki, or stress-reduction techniques, which may help with fatigue or stress.
With thoughtful planning and support, it’s possible to navigate the holidays in a way that prioritizes your well-being and still allows you to enjoy what’s meaningful.
by Bag It Team | Nov 8, 2023 | Educational Articles
Palliative and hospice care provide similar, but different services for patients and their families that focus on a holistic approach and their quality of life.
Palliative care is a way to help people with serious illnesses feel better physically and emotionally, and it can start at any point in their illness. It works with other types of treatments that aim to cure the illness. By contrast, hospice care is a special kind of palliative care for those with less than six months to live, with a main focus on keeping them comfortable and emotionally-supported during that time.
Here are some important differences between these two kinds of care:
Palliative Care
- Aims to reduce pain and suffering in people with serious illnesses.

Read more from the National Hospice and Palliative Care Organization
- Can start at any stage of the illness, including at diagnosis, and can coexist with treatments, regardless of the person’s expected recovery.
- Can take place in various locations, including hospitals, clinics, or even at home.
- The intensity of medical treatment can vary widely, potentially including strong treatments.
- Often covered by health insurance and integrated into regular medical care.
Hospice Care
- Primarily for individuals with a short life expectancy, often six months or less and involves a team of experts.
- Main goal is to provide maximum comfort rather than aiming for a cure.
- Usually provided at the patient’s home, in a specialized hospice facility, or in a hospital.
- Typically begins when it becomes clear that treatments are not effective, focusing on the patient’s comfort in their final days or months.
- Emphasizes comfort and symptom management, often discontinuing aggressive treatments.
- Often covered by Medicare, Medicaid, or private insurance for eligible patients.
Both palliative care and hospice care provide comfort and support for patients, one throughout cancer or other illness, and the other as one approaches the end of life. Have a conversation with your doctor to figure out the kind of care that’s right for you and your unique situation, so you can live your best life.
Don’t Wait! Bag It Bag and online resources are able to provide ways to empower patients and their families to ask for these services (palliative and hospice care) to improve the quality of life of patients and their families. Order a Bag and explore our Cancer Resource Center.
Additional Resources
by Bag It Team | Jul 7, 2022 | Podcasts
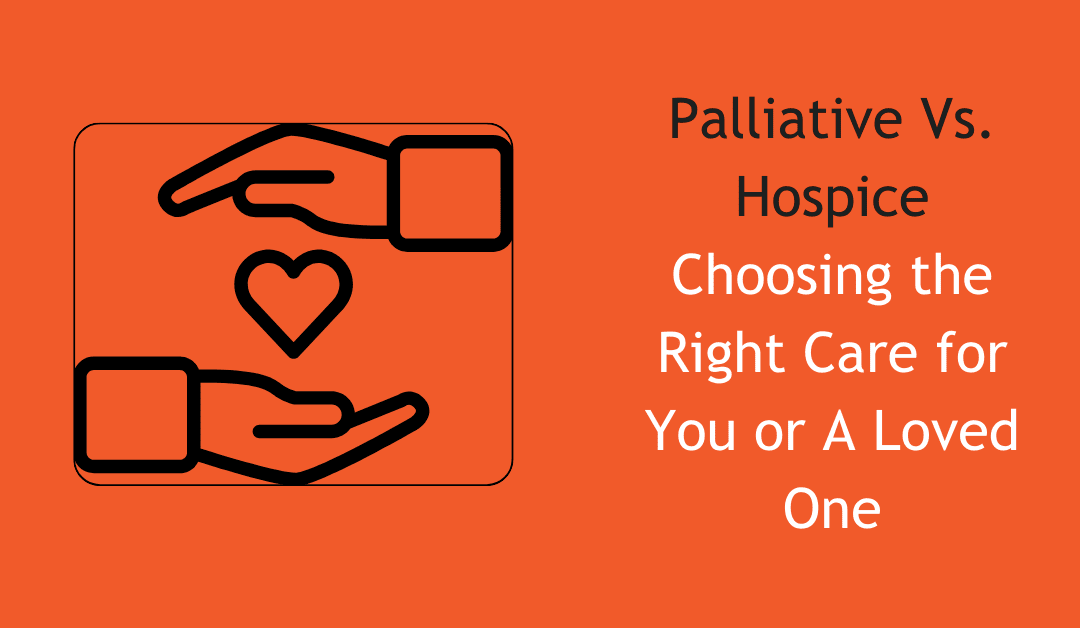
On this episode of Your Guide Through Cancer Podcast, Executive Director, Mindy Griffin speaks with Victoria Cramer, a three-time cancer survivor and an author, motivational speaker, happiness coach, and recovering global leader in the hotel industry. They explore some of the life hacks she discovered as she was surviving cancer. Victoria is a people champion and spends much of her time greening up the human spirit and mentoring the human race on how to find happiness in spite of the epic stuff thrown at us each day.

by Bag It Team | Oct 11, 2021 | Educational Articles
If you were diagnosed with a chronic illness such as cancer, heart disease, an autoimmune disease, or diabetes, experiencing a period of sadness, anxiousness, worry, anger, and stress is not uncommon. But if distressing symptoms persist after a couple of weeks, depression could be further complicating your overall health.
Possible signs of depression:
- Persistent sadness, tearfulness, emptiness, anxiousness
- Feeling hopeless, worthless, guilty, or pessimistic
- Irritability, outbursts of anger, frustration
- Feeling helpless
- Restlessness, loss of interest in pleasurable activities
- Lack of energy, fatigue
- Memory issues, difficulty with concentration or decision making
- Sleep disturbances (insomnia, oversleeping)
- Changes in your appetite or weight gain/loss
- Unexplained aches or pains
- Frequent thoughts of self-harm, death or suicide
The good news is that depression is highly treatable, and working with your healthcare team is the place to start on your path to wellness. As with any health condition, the earlier the treatment for depression begins the more effective it is.
Don’t wait for your healthcare provider to bring up the subject. As you prepare for your next appointment, make this one of your top three topics to discuss. Write down your depressive symptoms, how long you have had them, how often, intensity, etc. Be honest and describe their impact on your daily life and those around you.
Bring a complete list of all the medications (and supplements) you take. Also let the doctor know about any personal history of anxiety or depression in yourself or your family. (Remember that everything you share with your healthcare team is private and confidential. It cannot be discussed with others without your permission.)
Your healthcare provider will explore the treatment options with you. Depression is often effectively treated with medication, “talk therapy” (talking one-on-one with a professional), or both. Find what works for you. Be patient as it may take some time to feel better. Research has shown that treating your chronic illness and depression together can help you manage both more effectively and improve your overall quality of life.
Should you find yourself in a crisis, call the NAMI Helpline at 800-950-NAMI or text “NAMI” to 741741









Recent Comments