by Bag It Team | Feb 8, 2022 | Educational Articles
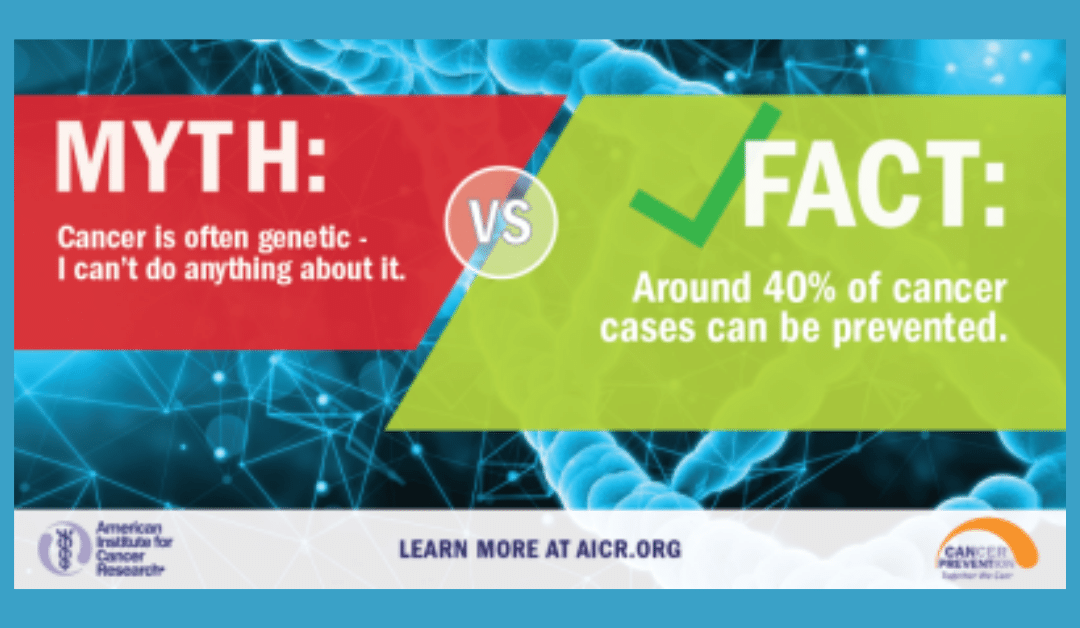
We wish we could say that all cancer is preventable if you just follow these steps, but that is not the case. However, research has shown that more than 40 percent of all cancers diagnosed can be attributed to preventable causes. That is why February is dedicated to cancer prevention.
Knowing the actions we need to take and actually taking them, does often require change in our lifestyle. Some of the actions we can take might feel a little easier such as not getting too much sun exposure, skipping the tanning bed, and making sure to have sun protection on when you are exposed. Some actions might feel more difficult like maintaining a healthy weight, quitting smoking, making different food choices and exercising regularly. A clean bill of health will show you the effort is worth it.

These behavior changes are listed as the top contributing factors for cancer prevention:
- Quit smoking: (this includes cigarettes, pipes, cigars, chewing tobacco and e-cigarettes) Tobacco use has been shown to increase the risk of developing 17 different types of cancer.
- Maintain a healthy weight: Being overweight or obese as an adult increases a person’s risk for 15 types of cancer. Talk to your doctor about what is a healthy weight for you.
- Be physically active: Being physically active reduces risk for nine types of cancer. Aim for at least 30 minutes of activity 5 times a week.
- Limit alcohol intake: Order smaller portions and drink a glass of water after every alcoholic beverage.
- Get regular screenings: American Cancer Society cancer screening guidelines by age.
- Get available vaccines: The Human papillomavirus (HPV) vaccine can significantly decrease the risk of several cancers including cervical, throat, tongue, anal, and other genital cancers. The Hepatitis B vaccine decreases the risk for liver cancer.
- Protect your skin from the sun: limit sun exposure between 10 a.m. and 4 p.m., make sure to wear sunscreen, clothing that covers your skin, and avoid tanning beds.
- Know your family history: Early detection can be key in life saving treatment. Knowing your family history can help you and your doctor plan for regular screenings (which may be recommended earlier with a known family history).
- Follow a healthy diet: AICR’s New American Plate, (⅔ whole grains, vegetables, fruit and beans, ⅓ protein), emphasizes foods that can reduce your risk for cancer and other chronic diseases.
There are lots of programs that can help you with weight maintenance, quitting smoking and alcohol intake. Talk to your doctor for any recommendations they feel might help. AICR’s website offers healthy recipes that contain cancer fighting foods.
If talking with your family about their health history feels difficult, practice with a friend first. Remind them that knowing their history can help you with early detection and prevention. If you do not have family available to ask about their history, talk to your doctor about genetic testing that may be available.
If getting started with activity is a little overwhelming or you don’t know what you like to do, many exercise programs have classes available online. If you find something you enjoy, you are much more likely to engage in activity regularly. Try lots of options and remember to start where you are.
In this month that focuses on LOVE, show yourself (and those who love you) some love by committing to lifestyle changes that will reduce your risk of being diagnosed with cancer. If you need a little extra support and accountability, you can take the pledge for AICR’s Click, Connect, and Commit campaign which offers a step-by-step guide to incorporate AICR’s 10 Cancer Prevention Recommendations in your everyday routine. You will also find a calendar with small steps you can take every day in February to help work towards your long term prevention goals.

by Bag It Team | Jan 12, 2022 | Educational Articles
 Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).
Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).
Whether you personally have cancer or not, genetic testing can be helpful for your situation. If you have a cancer that was caused by a mutation, genetic testing can provide important information about how to treat your cancer, as well as your risk for developing a second cancer.
If you have not been diagnosed with cancer, genetic testing can estimate the likelihood of being diagnosed with certain types of cancer in your lifetime. The test can tell you if you have a higher risk than most people of developing those cancers, but not that you will definitely be diagnosed.
Most cancers are caused by acquired (somatic) variants which occur spontaneously during a person’s lifetime, often due to lifestyle and environmental factors. These variants are not passed on to the next generation. Sometimes, cancers can be common in a family but are not due to an inherited gene mutation.
If you do have a genetic mutation, you and your family members can take steps to manage your cancer risks and health care. Children of parents with an inherited cancer mutation have a 50 percent chance of having the mutation themselves.
Discuss your individual circumstances and family history of cancer with your doctor. Seek their advice on whether you should be referred for genetic testing, and which tests to have. Testing is a complex decision on multiple levels, with implications for your family as well. A genetic counselor is highly recommended before and after testing as interpreting the test results can also be complicated.
For more information about genetic testing, please visit these websites.
by Mindy Griffith | Dec 9, 2021 | Educational Articles
Coping with cancer, Covid, or other health or life challenges can make it tough to remember our blessings during this season of giving, gratitude, and celebration we call “the holidays.”
But expressing gratitude goes beyond refocusing away from our challenges to simply find the goodness in our lives. Its power also enables us to accept the struggles that are present in our lives while also fostering resilience and hope – making it a practice worthy of adopting even during the most difficult of times.
Gratitude research finds links with stress relief, improved social ties/relationships, benefits to physical well being like better sleep, lower inflammation, blood pressure, and pain, as well a positive correlation with healthier lifestyle factors like diet and exercise.
Ongoing studies are being conducted to study the effects of what happens to the brain when a person practices gratitude. Findings suggest that it may help train the brain to be more sensitive to the experience of gratitude, which could contribute to lasting effects and improved mental health over time.
Your gratitude practice doesn’t have to be complicated. Adopting gratitude as part of your routine takes consistency and some time. You can be grateful for past, present or future blessings, and the more specific the entries, the better.
Write a thank you note or letter of appreciation to someone, then decide if you want to send it to the person. You don’t have to share it, though it might be a way to strengthen a relationship.
There are apps aplenty in the app stores if you want to record your entries digitally, and they even have reminders. Write in a journal, or simply and silently list three things you are thankful for as you lie in bed and drift off to sleep. Can’t stay awake long enough? Spend a few minutes in the morning before you get up and start your day. This can also be a good way to set an intention for the day. Gratitude, meditation and prayer are also methods of appreciating the joy in our lives. Use whatever works for you!

by Bag It Team | Oct 11, 2021 | Educational Articles
If you were diagnosed with a chronic illness such as cancer, heart disease, an autoimmune disease, or diabetes, experiencing a period of sadness, anxiousness, worry, anger, and stress is not uncommon. But if distressing symptoms persist after a couple of weeks, depression could be further complicating your overall health.
Possible signs of depression:
- Persistent sadness, tearfulness, emptiness, anxiousness
- Feeling hopeless, worthless, guilty, or pessimistic
- Irritability, outbursts of anger, frustration
- Feeling helpless
- Restlessness, loss of interest in pleasurable activities
- Lack of energy, fatigue
- Memory issues, difficulty with concentration or decision making
- Sleep disturbances (insomnia, oversleeping)
- Changes in your appetite or weight gain/loss
- Unexplained aches or pains
- Frequent thoughts of self-harm, death or suicide
The good news is that depression is highly treatable, and working with your healthcare team is the place to start on your path to wellness. As with any health condition, the earlier the treatment for depression begins the more effective it is.
Don’t wait for your healthcare provider to bring up the subject. As you prepare for your next appointment, make this one of your top three topics to discuss. Write down your depressive symptoms, how long you have had them, how often, intensity, etc. Be honest and describe their impact on your daily life and those around you.
Bring a complete list of all the medications (and supplements) you take. Also let the doctor know about any personal history of anxiety or depression in yourself or your family. (Remember that everything you share with your healthcare team is private and confidential. It cannot be discussed with others without your permission.)
Your healthcare provider will explore the treatment options with you. Depression is often effectively treated with medication, “talk therapy” (talking one-on-one with a professional), or both. Find what works for you. Be patient as it may take some time to feel better. Research has shown that treating your chronic illness and depression together can help you manage both more effectively and improve your overall quality of life.
Should you find yourself in a crisis, call the NAMI Helpline at 800-950-NAMI or text “NAMI” to 741741

by Bag It Team | Sep 14, 2021 | Educational Articles
Myth #1: Everyone experiences pain with cancer.
Facts:
- About half of people with cancer experience pain at some point – but about half don’t.
- Pain management is part of cancer treatment. In most cases pain can be controlled.
- Those with advanced cancer usually experience more pain than someone newly diagnosed.
Learn about the different types of pain, its causes, and how pain can be measured Causes of cancer pain: Pain can be caused by the tumor itself, cancer tests or procedures done, or it can occur as a side effect of treatment (surgery, chemotherapy, immunotherapy, radiation therapy). There can be more than one cause of pain. Some pain ends when treatment ends but some pain can be ongoing and chronic. Types of Pain:
- Acute pain – this type of pain comes on quickly but it does not last long. It can be mild, moderate, or severe.
- Chronic pain -this type of pain can be consistent or it can get worse, lasing a long time. Again, it can be mild, moderate, or severe.
- Breakthrough pain – this type of pain is usually a sudden increase in intense pain that “breaks through” the pain medications being taken to control pain, typically between does. It lasts for a short time. There are medications specifically used to treat this type of pain.
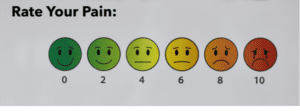
Pain Severity: Everyone experiences pain differently. It’s a good idea to keep a record of your pain to share with your healthcare team. Using one of the customizable logs in section 2 of Bag It’s My Companion Guidebook is an easy way to track your pain. You can use the scale below to assess your pain’s severity and type, noting when, where, how it feels (e.g. “burning,” “stabbing,” “throbbing) and other pertinent details on the form. Make copies to give to your healthcare team at your next appointment. This will help them to determine a pain management plan tailored just for you. Using a scale from “0” to “10”:
- 0 means no pain
- 1 to 3 means mild pain
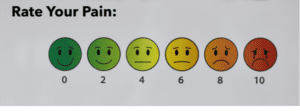
- 4 to 6 means moderate pain
- 7 to 10 means severe pain
Myth #2: Only opioid medications relieve cancer pain.
Facts:
- Non-opioid medications may be effective pain relievers depending on the type of pain someone is experiencing.
- Palliative surgery or radiation therapy is sometimes performed to ease symptoms and increase comfort.
- Palliative (supportive care) is care that focuses on relieving the symptoms of cancer, like pain, and other impacts on your physical, emotional, mental and spiritual well-being.
- Physical therapy, exercise, complementary and integrative medicine therapies such as acupuncture, massage and relaxation techniques are possible ways to manage pain without medication.
A personalized pain management plan prescribed by your healthcare team could include one or more of the above treatments to improve your quality of life. It’s important to talk openly with your healthcare team if you are experiencing pain. In addition to describing the pain in detail, let them know how it is impacting your daily life.
Palliative care (supportive care)
Palliative care is not hospice care. The aim of palliative, or supportive, care is to improve quality of life and maintain independence by reducing symptoms, managing pain, and supporting patients and their families. The aim of hospice care is to help the patient approach the end of life with peace, respect, and dignity, and it includes palliative care. Palliative care is an approach to care that addresses the person as a whole, not just their disease. The goal is to prevent or treat, as early as possible, the symptoms and side effects of the disease and its treatment, in addition to any related psychological, social, and spiritual problems. You can receive palliative care at any age and at any stage. Receiving palliative care does not mean that you will no longer receive treatment for the disease. People often receive treatment to slow, stop, or eliminate cancer in addition to treatment to ease discomfort. In fact, research shows that people who receive both types of treatment often have less severe symptoms, a better quality of life, and report they are more satisfied with treatment. Ask your healthcare team about the ways palliative care might be helpful to you and your family.
Additional Resources on Pain
ASCO Answers: Managing Cancer-Related Pain
Cancer Pain Control: Support for People With Cancer
ASCO’s booklet, Palliative Care
by Bag It Team | Aug 11, 2021 | Educational Articles
 August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
Did you know…
- About 25% of cancer deaths are from lung cancer – that’s more than colon, breast and prostate cancer deaths combined. (But the good news is that fewer Americans are smoking these days and new lung cancer treatments have been very effective in controlling some types of advanced disease.)
- Active cigarette smoking is by far the leading cause (about 80-90%) of lung cancer, but air pollution, secondhand smoke and other chemicals in the home and workplace, and family history, are also risk factors.
- While some experience symptoms related to the lungs, most people with lung cancer don’t have symptoms until the cancer is advanced.
- If you are at high risk*, an annual low-dose CT scan to screen for lung cancer may save your life. It can detect lung cancer earlier, when it is more treatable. Speak with your doctor about your personal health history and screening risks, as it is not recommended for everyone.

*(i.e. 1 pack a day for 20 years, 2 packs a day for 10 years, etc.)
Click here to order a lung cancer-specific or standard Bag it bag for yourself or as a gift for someone else. (available in English and Spanish)




 Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).
Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).


 August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
August 1st is World Lung Cancer Day, a day to raise awareness about lung health and how to prevent lung cancer.
Recent Comments