
Fighting Cancer Through Screening Legislation
Amy Cojanis, Bag It Cancer Administrative Services Manager, Mo Osife, Philanthropy/Advocacy Director for Cancer Support Communities of Arizona and Will Grove, Outreach Director of the Brain Injury Alliance of Arizona contributed to a guest editorial on how we can all come together to fight cancer through legislation. We are grateful to these writers and organizations as well as to Arizona co-sponsors like @SenatorSinema @RepRaulGrijalva @RepCiscomani for working to push multi-cancer screening legislation. Read our op-ed on the issue.

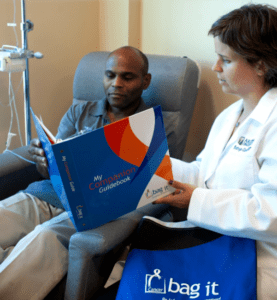 KGUN 9 News Anchor and Reporter Pat Parris Interviews colon cancer survivor Ingrid Jacobs and Bag It Cancer’s Executive Director Mindy Griffith about the impact the resources in the Bag It Bag have had on cancer patients. Every month KGUN 9 features a local nonprofit for our Giving Project and Bag It is their charity for the month of February, 2023.
KGUN 9 News Anchor and Reporter Pat Parris Interviews colon cancer survivor Ingrid Jacobs and Bag It Cancer’s Executive Director Mindy Griffith about the impact the resources in the Bag It Bag have had on cancer patients. Every month KGUN 9 features a local nonprofit for our Giving Project and Bag It is their charity for the month of February, 2023.



 Bag It Cancer’s Executive Director Mindy Griffith’s editorial about the forward movement of the Medicare Multi-Cancer Early Detection Screening Coverage Act is featured in the Arizona Daily Star on October 6, 2022. In it, she praises the seven bipartisan members of the U.S. House–including two members from Arizona’s Congressional leadership–for endorsing this impactful legislation that would ensure Medicare is able to provide coverage for early cancer detection tools.
Bag It Cancer’s Executive Director Mindy Griffith’s editorial about the forward movement of the Medicare Multi-Cancer Early Detection Screening Coverage Act is featured in the Arizona Daily Star on October 6, 2022. In it, she praises the seven bipartisan members of the U.S. House–including two members from Arizona’s Congressional leadership–for endorsing this impactful legislation that would ensure Medicare is able to provide coverage for early cancer detection tools.

Recent Comments