by Bag It Team | Feb 8, 2022 | Educational Articles
We wish we could say that all cancer is preventable if you just follow these steps, but that is not the case. However, research has shown that more than 40 percent of all cancers diagnosed can be attributed to preventable causes. That is why February is dedicated to cancer prevention.
Knowing the actions we need to take and actually taking them, does often require change in our lifestyle. Some of the actions we can take might feel a little easier such as not getting too much sun exposure, skipping the tanning bed, and making sure to have sun protection on when you are exposed. Some actions might feel more difficult like maintaining a healthy weight, quitting smoking, making different food choices and exercising regularly. A clean bill of health will show you the effort is worth it.

These behavior changes are listed as the top contributing factors for cancer prevention:
- Quit smoking: (this includes cigarettes, pipes, cigars, chewing tobacco and e-cigarettes) Tobacco use has been shown to increase the risk of developing 17 different types of cancer.
- Maintain a healthy weight: Being overweight or obese as an adult increases a person’s risk for 15 types of cancer. Talk to your doctor about what is a healthy weight for you.
- Be physically active: Being physically active reduces risk for nine types of cancer. Aim for at least 30 minutes of activity 5 times a week.
- Limit alcohol intake: Order smaller portions and drink a glass of water after every alcoholic beverage.
- Get regular screenings: American Cancer Society cancer screening guidelines by age.
- Get available vaccines: The Human papillomavirus (HPV) vaccine can significantly decrease the risk of several cancers including cervical, throat, tongue, anal, and other genital cancers. The Hepatitis B vaccine decreases the risk for liver cancer.
- Protect your skin from the sun: limit sun exposure between 10 a.m. and 4 p.m., make sure to wear sunscreen, clothing that covers your skin, and avoid tanning beds.
- Know your family history: Early detection can be key in life saving treatment. Knowing your family history can help you and your doctor plan for regular screenings (which may be recommended earlier with a known family history).
- Follow a healthy diet: AICR’s New American Plate, (⅔ whole grains, vegetables, fruit and beans, ⅓ protein), emphasizes foods that can reduce your risk for cancer and other chronic diseases.
There are lots of programs that can help you with weight maintenance, quitting smoking and alcohol intake. Talk to your doctor for any recommendations they feel might help. AICR’s website offers healthy recipes that contain cancer fighting foods.
If talking with your family about their health history feels difficult, practice with a friend first. Remind them that knowing their history can help you with early detection and prevention. If you do not have family available to ask about their history, talk to your doctor about genetic testing that may be available.
If getting started with activity is a little overwhelming or you don’t know what you like to do, many exercise programs have classes available online. If you find something you enjoy, you are much more likely to engage in activity regularly. Try lots of options and remember to start where you are.
In this month that focuses on LOVE, show yourself (and those who love you) some love by committing to lifestyle changes that will reduce your risk of being diagnosed with cancer. If you need a little extra support and accountability, you can take the pledge for AICR’s Click, Connect, and Commit campaign which offers a step-by-step guide to incorporate AICR’s 10 Cancer Prevention Recommendations in your everyday routine. You will also find a calendar with small steps you can take every day in February to help work towards your long term prevention goals.

by Bag It Team | Jan 1, 2022 | Podcasts
Your Guide Through Cancer podcast host, Bag It Executive Director, Mindy Griffith interviews Stage 4 Cancer Survivor and Advocate Sheila McGlown. A wonderful example of what Bag It can do for you or your loved ones during this trying and worrying time. Join Mindy for this uplifting story.
Sheila uses her voice to raise awareness about the racial disparities faced by black women throughout their breast cancer journey. Receiving a breast cancer diagnosis is devastating for anyone, and Sheila passionately believes that racial disparities should not have an impact on the standard of treatment that black women receive.

by Bag It Team | Oct 11, 2021 | Educational Articles
If you were diagnosed with a chronic illness such as cancer, heart disease, an autoimmune disease, or diabetes, experiencing a period of sadness, anxiousness, worry, anger, and stress is not uncommon. But if distressing symptoms persist after a couple of weeks, depression could be further complicating your overall health.
Possible signs of depression:
- Persistent sadness, tearfulness, emptiness, anxiousness
- Feeling hopeless, worthless, guilty, or pessimistic
- Irritability, outbursts of anger, frustration
- Feeling helpless
- Restlessness, loss of interest in pleasurable activities
- Lack of energy, fatigue
- Memory issues, difficulty with concentration or decision making
- Sleep disturbances (insomnia, oversleeping)
- Changes in your appetite or weight gain/loss
- Unexplained aches or pains
- Frequent thoughts of self-harm, death or suicide
The good news is that depression is highly treatable, and working with your healthcare team is the place to start on your path to wellness. As with any health condition, the earlier the treatment for depression begins the more effective it is.
Don’t wait for your healthcare provider to bring up the subject. As you prepare for your next appointment, make this one of your top three topics to discuss. Write down your depressive symptoms, how long you have had them, how often, intensity, etc. Be honest and describe their impact on your daily life and those around you.
Bring a complete list of all the medications (and supplements) you take. Also let the doctor know about any personal history of anxiety or depression in yourself or your family. (Remember that everything you share with your healthcare team is private and confidential. It cannot be discussed with others without your permission.)
Your healthcare provider will explore the treatment options with you. Depression is often effectively treated with medication, “talk therapy” (talking one-on-one with a professional), or both. Find what works for you. Be patient as it may take some time to feel better. Research has shown that treating your chronic illness and depression together can help you manage both more effectively and improve your overall quality of life.
Should you find yourself in a crisis, call the NAMI Helpline at 800-950-NAMI or text “NAMI” to 741741

by Bag It Team | Sep 14, 2021 | Educational Articles
Myth #1: Everyone experiences pain with cancer.
Facts:
- About half of people with cancer experience pain at some point – but about half don’t.
- Pain management is part of cancer treatment. In most cases pain can be controlled.
- Those with advanced cancer usually experience more pain than someone newly diagnosed.
Learn about the different types of pain, its causes, and how pain can be measured Causes of cancer pain: Pain can be caused by the tumor itself, cancer tests or procedures done, or it can occur as a side effect of treatment (surgery, chemotherapy, immunotherapy, radiation therapy). There can be more than one cause of pain. Some pain ends when treatment ends but some pain can be ongoing and chronic. Types of Pain:
- Acute pain – this type of pain comes on quickly but it does not last long. It can be mild, moderate, or severe.
- Chronic pain -this type of pain can be consistent or it can get worse, lasing a long time. Again, it can be mild, moderate, or severe.
- Breakthrough pain – this type of pain is usually a sudden increase in intense pain that “breaks through” the pain medications being taken to control pain, typically between does. It lasts for a short time. There are medications specifically used to treat this type of pain.
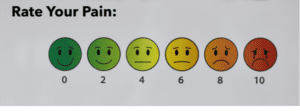
Pain Severity: Everyone experiences pain differently. It’s a good idea to keep a record of your pain to share with your healthcare team. Using one of the customizable logs in section 2 of Bag It’s My Companion Guidebook is an easy way to track your pain. You can use the scale below to assess your pain’s severity and type, noting when, where, how it feels (e.g. “burning,” “stabbing,” “throbbing) and other pertinent details on the form. Make copies to give to your healthcare team at your next appointment. This will help them to determine a pain management plan tailored just for you. Using a scale from “0” to “10”:
- 0 means no pain
- 1 to 3 means mild pain
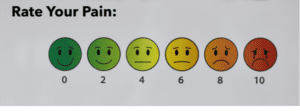
- 4 to 6 means moderate pain
- 7 to 10 means severe pain
Myth #2: Only opioid medications relieve cancer pain.
Facts:
- Non-opioid medications may be effective pain relievers depending on the type of pain someone is experiencing.
- Palliative surgery or radiation therapy is sometimes performed to ease symptoms and increase comfort.
- Palliative (supportive care) is care that focuses on relieving the symptoms of cancer, like pain, and other impacts on your physical, emotional, mental and spiritual well-being.
- Physical therapy, exercise, complementary and integrative medicine therapies such as acupuncture, massage and relaxation techniques are possible ways to manage pain without medication.
A personalized pain management plan prescribed by your healthcare team could include one or more of the above treatments to improve your quality of life. It’s important to talk openly with your healthcare team if you are experiencing pain. In addition to describing the pain in detail, let them know how it is impacting your daily life.
Palliative care (supportive care)
Palliative care is not hospice care. The aim of palliative, or supportive, care is to improve quality of life and maintain independence by reducing symptoms, managing pain, and supporting patients and their families. The aim of hospice care is to help the patient approach the end of life with peace, respect, and dignity, and it includes palliative care. Palliative care is an approach to care that addresses the person as a whole, not just their disease. The goal is to prevent or treat, as early as possible, the symptoms and side effects of the disease and its treatment, in addition to any related psychological, social, and spiritual problems. You can receive palliative care at any age and at any stage. Receiving palliative care does not mean that you will no longer receive treatment for the disease. People often receive treatment to slow, stop, or eliminate cancer in addition to treatment to ease discomfort. In fact, research shows that people who receive both types of treatment often have less severe symptoms, a better quality of life, and report they are more satisfied with treatment. Ask your healthcare team about the ways palliative care might be helpful to you and your family.
Additional Resources on Pain
ASCO Answers: Managing Cancer-Related Pain
Cancer Pain Control: Support for People With Cancer
ASCO’s booklet, Palliative Care

by Mindy Griffith | Apr 8, 2021 | Educational Articles
Bag It. Guiding one through cancer.
 So, it’s National Read a Roadmap week, and I love a bizarre holiday that connects to many things I love and makes me smile. First, I recall being on a road trip a few years ago, and yes we had GPS on our phones and were using that, when we were trying to find maps of the area we were in just because (okay maybe I wanted to use them later to scrapbook the adventure). At the 3rd gas station we found one, it was dated and covered in dust and the employees thought my friend was crazy for wanting one but we were thrilled!
So, it’s National Read a Roadmap week, and I love a bizarre holiday that connects to many things I love and makes me smile. First, I recall being on a road trip a few years ago, and yes we had GPS on our phones and were using that, when we were trying to find maps of the area we were in just because (okay maybe I wanted to use them later to scrapbook the adventure). At the 3rd gas station we found one, it was dated and covered in dust and the employees thought my friend was crazy for wanting one but we were thrilled!
Then a friend was visiting me and in the side panel of my car I have a few maps, because you never know when you might need one. She found this hilarious and took a picture of it to post on social media asking people if they even knew what they were – she couldn’t believe that I had them in my car. (FYI: I have used them from time to time.)
Now I love technology and frequently use digital maps, but it’s always good to have a back-up plan as we know that technology doesn’t work everywhere or your might not have your phone charged or maybe you just appreciate having things in a printed format. Print makes things easier to share and more readily available (but I encourage you to order those maps in advance of your next trip).
 How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
Reading a roadmap takes some practice, just like understanding cancer. The Bag It bag works as a guide to help those impacted by cancer understand more about their diagnosis and cope with the bumps along the way. When you receive a cancer diagnosis you don’t get the map (digital or print) to go with it. You don’t know the vocabulary, the questions to ask, which treatment to take, or which exit has a support network. You need something to help familiarize you with this experience. Your healthcare team is one guide and a Bag It bag is another valuable guide.
The take-everywhere binder (yep, even on that road trip) helps organize appointments and records (similar to your brochures and itineraries). The booklets provide coping tips, support information, reliable cancer information and questions to ask. It’s all in the bag! You won’t feel lost during or after treatment with Bag It as your guide.
Bag It wants to ensure anyone who wants or needs a bag has them available to them. You can order one as a gift for someone when they are diagnosed with cancer to help them cope or you can order/request one for yourself. They are a doctor-recommended resource for anyone with any type of cancer.
If you don’t currently know anyone who could benefit consider participating in our Spring 2021 Fundraiser – Gift a Bag It Bag. With a $41 contribution you can help provide a source of comfort and the printed navigation tools to help a patient throughout their cancer treatment and beyond.










 So, it’s
So, it’s  How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
How does reading a map and my random stories (that made me smile with the memories) connect to cancer and Bag It?
Recent Comments