
by Bag It Team | Jul 12, 2022 | Educational Articles
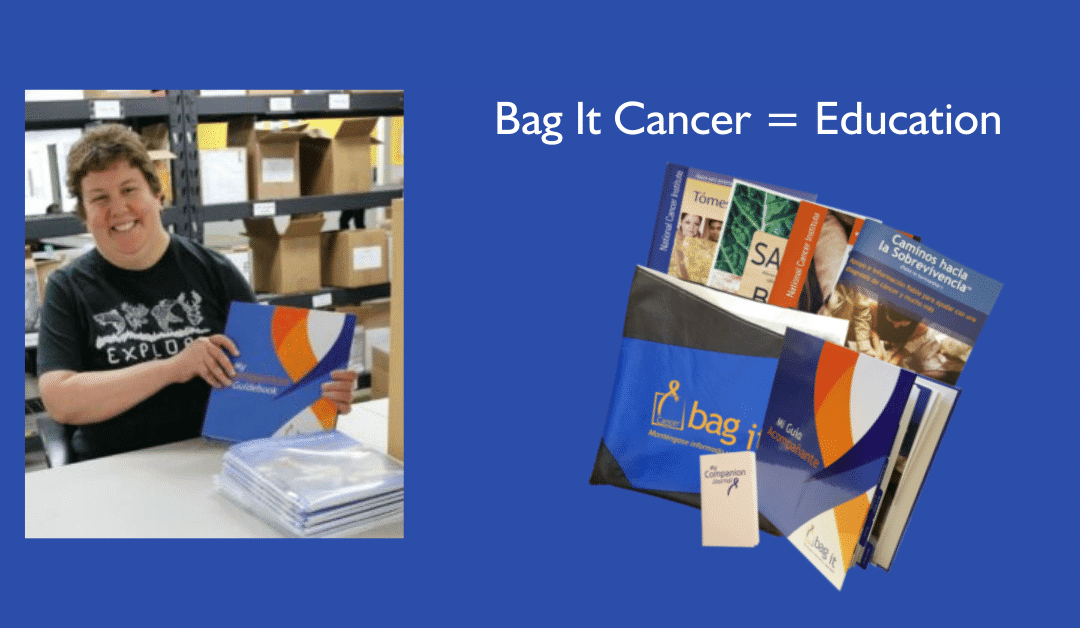
Every 18 to 24 months, we gather a committee of cancer survivors, care partners, oncology care providers, and nonprofit partners to conduct a review of the Bag It Bag. They assess how the current bag content and design are meeting the needs of people with cancer, their care partners, families, and the healthcare providers who care for them. The group also considers how the Bag could be improved.
The feedback we received from our recent review was thoughtful and insightful, as always. The consensus was that the significant revisions made to the Bag in 2019 continue to benefit the quality of the materials. Some helpful suggestions on ways to refresh and enhance some of the content were also offered.
The Covid-19 pandemic did not prevent us from completing this important process or continuing our work. For the Bag It Team, the challenges it brought reinforced that this valuable resource is critical for those dealing with cancer, renewing our commitment to our mission of educating, supporting, and empowering those impacted by cancer.
2022 Bag It Bag Updates
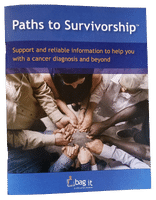
Paths to Survivorship Booklet
We added new information about dealing with potential cancer treatment side effects such as hot flashes, bone health, and genital and urinary problems, which are common for some types of cancer. It is important for people to understand all of their rights and options to best navigate their situations related to work, disability and health insurance, and managing finances. Triage Cancer provided valuable content on these legal and practical issues.
 An overview about genetic and biomarker testing explains what they are and, when ordered by your doctor, how the test results can help your cancer care team offer you the most tailored options for effective treatment of your cancer. Your doctor will determine if this type of testing is appropriate for you.
An overview about genetic and biomarker testing explains what they are and, when ordered by your doctor, how the test results can help your cancer care team offer you the most tailored options for effective treatment of your cancer. Your doctor will determine if this type of testing is appropriate for you.
This booklet includes helpful lists of questions you can ask your healthcare team based on where you are in your diagnosis and treatment:
- Questions to ask your healthcare team about your diagnosis
- Questions to ask your healthcare team about cancer treatment
- Questions to ask your healthcare team about follow-up care
- Questions to ask your healthcare team about late and long-term side effects
- Questions to ask your healthcare team about living with chronic or advanced cancer
Here are printable versions of the questions to take with you to your appointments. You’ll also find other Self-Advocacy Tips and A Survivorship Checklist.
Paths to Survivorship (and all the booklets and forms in the bag) can be downloaded for free on our website. Want to share this great publication with others? You can email it in PDF format or send them the link to the Bag it Bag.
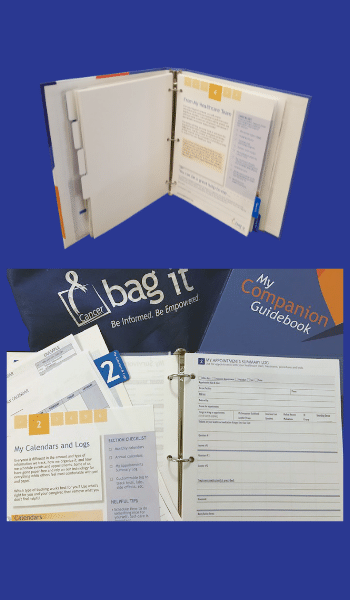
My Companion Guidebook
It goes without saying that there’s a lot of information coming your way when you or someone close to you is diagnosed with cancer. It can be overwhelming. A great deal of paperwork is given to you by your providers, and there is much to keep track of in an accurate and consistent manner.
 My Companion Guidebook is a helpful way to organize everything in one place to ensure you have access to what you need, when you need it. We’ve made some tweaks to make it easier to sort and store your records in the various sections, and added more tips on how to make the most of your appointments. There’s also a handy new page to keep a running list of your questions for your next doctor visit.
My Companion Guidebook is a helpful way to organize everything in one place to ensure you have access to what you need, when you need it. We’ve made some tweaks to make it easier to sort and store your records in the various sections, and added more tips on how to make the most of your appointments. There’s also a handy new page to keep a running list of your questions for your next doctor visit.
Blank copies of the forms to print or the fillable PDF format can be found on our Bag It Bag page.
Resources, Resources, and More Resources!
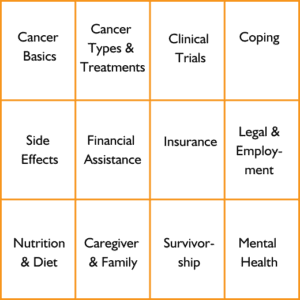
Did you know Bag It’s online Resource Center houses over 150 vetted websites covering a wide range of cancer topics? Whether you want education about your cancer type or to find support services out there that can help you or your family along the way, we’ve done the legwork to save you time and to bring you resources you can rely on.
At the same time, we also realize that not everyone has equal access to or is as comfortable using the internet. That’s why we added two new pages to My Companion Guidebook listing many helpful organizations to assist with some of the most common and pressing needs that cancer can bring. (Phone numbers are also listed in case you prefer to call and speak to someone there.)
Topics include:
To order a Bag It Bag for yourself or someone else, visit our Bag It Bag order page.
by Bag It Team | Jun 14, 2022 | Educational Articles
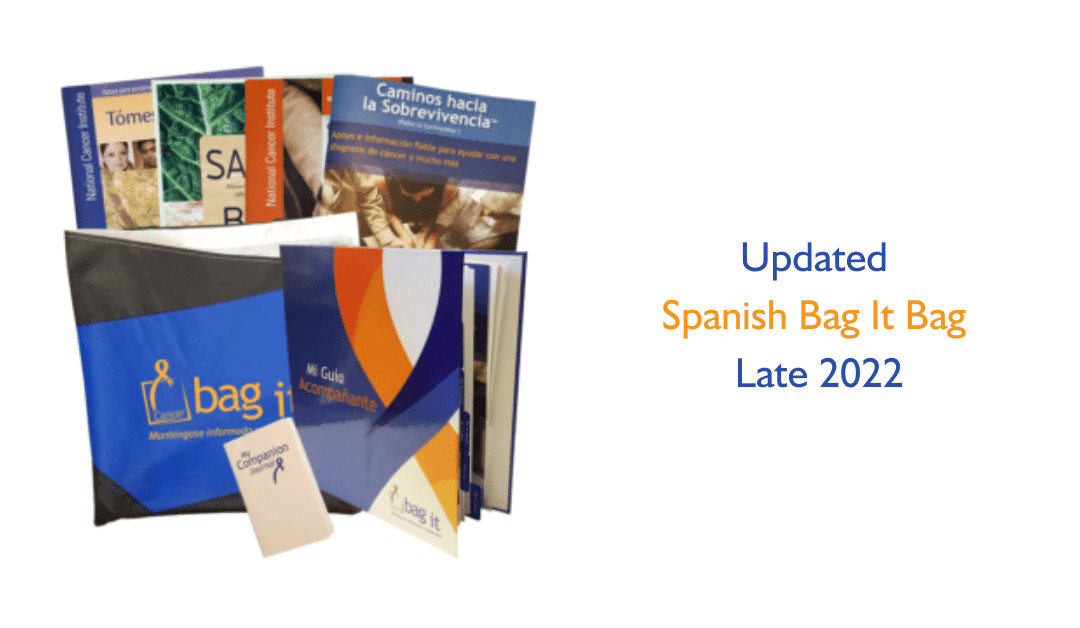
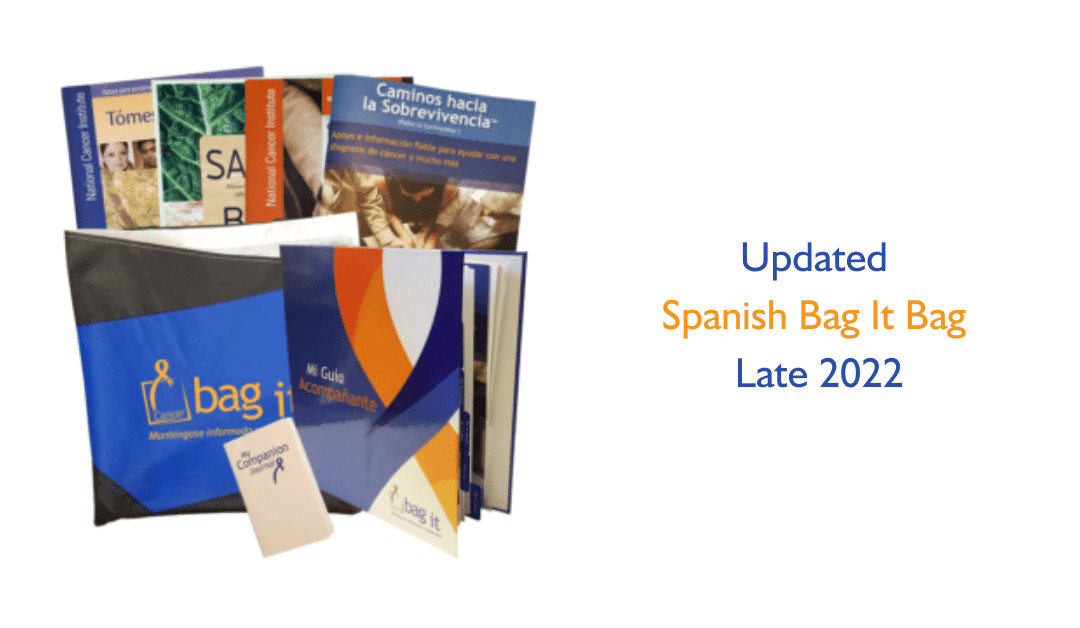
Bag It Cancer continually reviews the Bag to ensure it is as helpful as it can be for those living with cancer. This spring we conducted research through a series of interviews and focus groups of Latino and Hispanic survivors, caregivers and other stakeholders for input on how to better address their values, beliefs, language, and culture in the Spanish Bag.
We heard about a variety of topics that would be beneficial to include in the Spanish Bag, or address in a different way in the Bag.

For example, to many people, cancer=death. If someone is diagnosed with cancer, the only possible outcome is death. We hope to dispel this commonly-held misconception and others by educating Bag users and families about the evidence-based facts about cancer. We gained more insight about the importance of family in the Latino and Hispanic communities. Family members often take part in the decision making about treatment. Their involvement in that process, and as caregivers, can have huge impacts on a patient’s wellbeing.
We also learned that if nutritional information in the Bag isn’t tailored to culturally relevant foods, patients and caregivers may not make necessary changes to their diet during and after treatment. We plan to include recipes from Latina kitchens that adapt favorite Latin dishes to make them healthier – lower in fat, richer in fiber and vitamins, but still tasty.
Latinos and Hispanics are disproportionately affected by poor conditions of daily life which are shaped by a variety of structural and social position factors (such as income, education, occupations, cultural values, and social support systems), known as social determinants of health. These factors impact their cancer care and survival. We can’t overcome all of these barriers, but we can do our small part by educating and guiding Latinos and Hispanics with a more culturally-tailored Bag It Bag.
We look forward to introducing the new bicultural Bag It Bag to you and your patients at the end of the year.

by Bag It Team | Jun 14, 2022 | Educational Articles
Every cancer patient deserves the best care possible. There isn’t a provider on the planet who disagrees with that. For many cancer centers and health systems, the best means putting together an all-star team capable of meeting the full needs of the patient, including “financial, psychological, social, logistical or related to communication.” That is why no oncology team is complete without an Oncology Nurse Navigator.
An Oncology Nurse Navigator is a clinically trained individual (typically a professional RN with oncology-specific clinical knowledge) who offers individualized assistance to patients and caregivers to help address barriers to timely and appropriate cancer treatment. They advocate for their patients throughout the cancer care continuum from diagnosis through survivorship and coordinate all components involved in cancer care, including surgical, medical, and radiation oncologists; social workers; patient education; community support; financial and insurance assistance; etc. They perform a vital role on the patient’s cancer care team.
Bringing on an Oncology Nurse Navigator is the first step. Equipping them with the best tools available is the second. That is why so many providers turn to Bag It Cancer. Oncology Nurse Navigators can assist patients with various issues beyond healthcare; comprehensive patient education tools like Bag It matter a lot in these situations. By providing a Bag It Bag, an Oncology Nurse Navigator can also help a patient learn to advocate for themselves and introduce them to reliable information that can often be difficult to find.
”When meeting patients for the first time, we often find the devastation of the new Cancer diagnosis to be overwhelming. They are not sure who to turn to, or where to begin. As certified Nurse Navigators, our first meeting is a cornerstone for care needs and coordination.
Having the Bag It Bag helps to introduce our ability to support and stabilize the care they need. At the same time, we use it to education them in essential ways. Lastly, it is a place to keep things from getting misplaced, and helps keep the Cancer ‘in its place’ in their lives from the start.”
Anyone that has ever met with an Oncology Nurse Navigator knows that support like patient education matters a lot and can be the difference between a good and bad experience for patients and caregivers.
So, if you don’t already have an Oncology Nurse Navigator on your team, or are interested in becoming a certified navigator, reach out to our friends at the Academy of Oncology Nurse & Patient Navigators (AONN).
If your practice needs to upgrade your patient education materials to match your new all-star team, please reach out at cj@bagitcancer.org and learn how Bag It can enhance your practice.
by Bag It Team | Jun 14, 2022 | Educational Articles
For many patients, except for a fellow cancer survivor, no one other than their healthcare provider understands how devastating a cancer diagnosis can be. When worry or smiles turn to fear, anger, or sadness, providers are there.
While some providers have long recognized the value of providing comprehensive patient education materials, others have missed the mark by giving little to none, placing the burden on patients to find their own resources or information. When implemented correctly, patient education goes beyond informing patients about their cancer and treatment. It can play a crucial role in helping patients cope better, learn how to become a self-advocate, and how to be engaged in their care.
At Bag It Cancer, we believe patient education is primarily the provider’s responsibility. Most Bag recipients receive their Bag It Bags directly from their providers, ensuring that they’re receiving the trusted information at the right time. So yes, please continue to give your patients the Bag It Bag if you are a current Bag distributor. If you are not, consider how offering this critical aspect of patient care benefits both patients and clinicians.
Studies show that patient education can help patients be more informed, more engaged in their care, better equipped to ask better questions, more compliant with treatment, and enjoy a better quality of life. Providers who directly provide quality education materials like the Bag It Bag can be confident that their patients are accessing reliable information rather than obtaining misinformation that could be dangerous.
Ideally, here is what a patient education session for a newly-diagnosed patient would look like:
A provider walks in with a Bag It Bag and opens it up to introduce it to the patient. The patient, having been informed of their diagnosis, opens My Companion Guidebook to section 1 (My Personal Details) to see that the provider has already written in the details of their current diagnosis. The provider shows them copies of their recent scans and lab work which have already been added to the appropriate sections and discusses the results and next steps. The patient would also be directed to one of the booklets that the provider feels would be most helpful to them at that time. Now a difficult appointment where many patients often leave dazed and confused has become one where the patient leaves feeling cared for, prepared, empowered, and with a better sense of what to expect.
If you or your team are interested in seeing how Bag It can improve your oncology patient education services, please feel free to reach out at crispin@bagitcancer.org or call 520-337-2800.
by Bag It Team | May 10, 2022 | Educational Articles
We all know that a cancer diagnosis can be life-changing for everyone. Its impact isn’t just reserved to the physical changes experienced by patients, but also the mental health toll it can have on patients, families, friends, and entire communities. In recognition of Mental Health Awareness Month, our team at Bag It would like to share some helpful tips for you and your loved ones to ease your journey to survivorship.
Change your environment (even for a short while)
Take a vacation with a loved one. Vacations offer many mental health benefits, including reducing depression and anxiety. Your vacation doesn’t need to be extensive; even a weekend road trip can help reduce stress. A study found that “a short, three-day leisure trip reduced perceived levels of stress and reduced levels of the ‘stress hormone’ cortisol.” Another option is to take some time to enjoy nature. A 15-30 minute walk outside offers a chance to get some fresh air and reset. Maybe a stroll at the park or a hike on a trail might do the trick.
Take advantage of support programs in your community
Support groups are a safe, confidential space to share experiences and connect with others navigating similar challenges. They are often available in person or virtual, and you may find one at a local religious group, cancer center, or local cancer nonprofit. Studies have shown that attending a support group can lead to a better quality of life due to improved mood, self-image, and increased coping ability.
Take some time to count sheep
Sleep plays a vital role in how our bodies recover. A lack of adequate sleep has previously been thought to result from depression, but “growing evidence suggests that poor sleep may induce or exacerbate depression.” Inadequate sleep can also lead to anxiety disorders and may become an added source of worry and hyperarousal, which is a key contributor to insomnia. So find a bedtime each day that works for you. Wind down with some relaxation techniques as part of your bedtime routine and maximize comfort with a great mattress, pillow, and bedding. Your body will thank you for it.
Let’s get physical
Exercise offers so many benefits beyond just building muscle and burning calories. Moderate exercise “relieves stress, improves memory, helps you sleep better, and boosts your overall mood.” No matter your age or fitness level, 30-minutes of moderate exercise five times a week can make a lot of difference. You`ll feel more relaxed and see a change in your self-image. Physical activity is also essential for managing some of the side effects of cancer, including fatigue, weight loss, weight gain, and cardiovascular issues. It also plays a role in survivorship by reducing inflammation and joint pain.
Additional information can be found in the booklet Living Well with Cancer and Beyond. So find a fun activity that works for you, and get started today!
Form your squad
People face so many challenges daily, and these challenges get even more complex after a cancer diagnosis. It’s natural for people to retreat alone and deal in silence, but it’s not always the healthiest route. Find family members or close friends you trust as members of your support network. Social interactions are good for our overall physical and mental health. Cancer doesn’t have to be the focus of every conversation, and you have the right to determine what you feel comfortable sharing with others. A laugh with friends or dinner at your favorite restaurant can also offer a greater sense of well-being and relieves pent-up stress or pain.
Talk to your provider
It’s ok not to be ok. You are not alone. If the challenges around you become overwhelming or you find yourself in a dark place, never be ashamed to seek help. Talk to your provider or find a licensed mental health professional near you. If you have insurance, you can often find a provider in your network by visiting your insurance plan’s website. You can also visit the Bag It Resource Center to find reliable resources.
If you or someone you know is struggling with suicidal thoughts, please contact the National Suicide Prevention Lifeline. They are available 24 hours a day, everyday, Call: 1-800-273-8255 or Text: “HELLO” to 741741

by Bag It Team | Apr 12, 2022 | Educational Articles
Be prepared for every visit.
Manage your healthcare better.
April is National Records and Information Management Month! Keeping comprehensive and accurate medical records can empower you and your healthcare team to make the best decisions for your care.
So much of what we do for our health happens outside clinical settings. When you can track appointments, tests, nutrition and more over time, you and your healthcare team will have the right information and tools to manage your health. And, bonus, you will be more engaged in your overall care and prepared for each healthcare visit. Every detail stored and provided is vital because all the accumulated information can contribute to proper diagnosis, treatment, and follow-up care.
In honor of this month, Bag It would like to share a few tips to help you be great at your healthcare records and information management. And to show you the perfect tool to keep everything organized in one place, we give you a look at My Companion Guidebook.
Request copies of all your medical records and test results to store in one of Bag It’s tools, My Companion Guidebook. You can refer back to them and provide a backup copy if they get lost or are not accessible by a different healthcare provider.
Most providers use various electronic health records systems that are not compatible and don’t share your information between them. By keeping accurate copies of all lab work, treatment plans, etc., you can help manage the flow of information from providers and improve the quality of care.
Additionally, Bag It’s My Companion Guidebook (see portals page) will help you juggle the various usernames and passwords for different patient portals.
Use the My Appointments Summary Log in My companion Guidebook to write down your questions in advance of appointments. Make sure you fully understand what you are being told then write down the answers provided and any other notes on what was discussed during the appointment. Make sure you understand next steps needed for follow up care, next appointment, etc.
Sometimes, it can be tricky remembering everything discussed with your doctor. Take notes and/or ask if you can make a recording. Save the recording and notes by appointment dates for review later. This can help you remember what you talked about and be a quick reference material for family and friends.
Bag It’s My Companion Guidebook–The Perfect Tool To Keep You Organized
Use My Companion Guide to store medical info, healthcare and personal contacts, reports/scans/labs, calendar items, insurance info, notes and questions for the doctor, track side effects and symptoms, etc.
Maintaining this information and all the paperwork on an ongoing basis will make this an easy go-to reference for you, caregivers and family, and doctor visits.
The easy-to-use forms can be filled in by hand or use the fillable PDF format found on our website to print, save, and update later and share electronically with others as you see fit.

 An overview about genetic and biomarker testing explains what they are and, when ordered by your doctor, how the test results can help your cancer care team offer you the most tailored options for effective treatment of your cancer. Your doctor will determine if this type of testing is appropriate for you.
An overview about genetic and biomarker testing explains what they are and, when ordered by your doctor, how the test results can help your cancer care team offer you the most tailored options for effective treatment of your cancer. Your doctor will determine if this type of testing is appropriate for you. My Companion Guidebook is a helpful way to organize everything in one place to ensure you have access to what you need, when you need it. We’ve made some tweaks to make it easier to sort and store your records in the various sections, and added more tips on how to make the most of your appointments. There’s also a handy new page to keep a running list of your questions for your next doctor visit.
My Companion Guidebook is a helpful way to organize everything in one place to ensure you have access to what you need, when you need it. We’ve made some tweaks to make it easier to sort and store your records in the various sections, and added more tips on how to make the most of your appointments. There’s also a handy new page to keep a running list of your questions for your next doctor visit.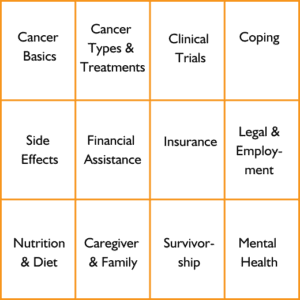





Recent Comments