by Bag It Team | Feb 8, 2023 | Educational Articles
Some good news about cancer…
It is estimated that nearly half of cancer deaths worldwide can be prevented, according to recently published medical research. Some cancers are out of our control, but we can make choices about our habits and the way we live to reduce our risk of cancer. Here are some examples:
- Don’t use tobacco
- Protect your skin from the sun
- Eat a plant-based diet
- Limit alcohol
- Maintain a healthy weight and move, move, move
- Get vaccinated against HPV and hepatitis B
- Practice safer sex and avoid risky behaviors
- Reduce your exposure to indoor and outdoor air pollution
Finally, know your family medical history and share it with your doctors. Most people do not have a family history of cancer so getting the cancer screenings your doctors recommend for your particular situation is important. Early detection can lead to better outcomes.
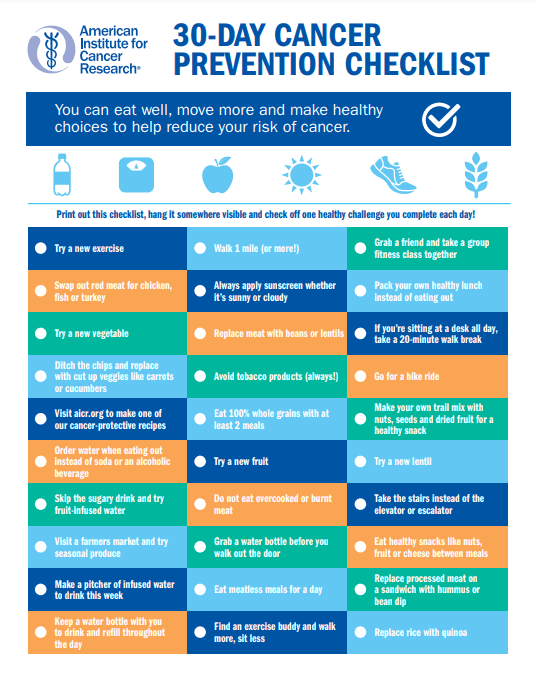
The American Institute for Cancer Research offers a free 30-day checklist to help you eat well, move more and make healthy lifestyle choices to reduce your cancer risk. Find it here along with other cancer prevention resources.
by Bag It Team | Dec 14, 2022 | Educational Articles
With all the medical advances and education for cancer, it is amazing that myths and misconceptions about cancer still abound and worry us needlessly.
Here we debunk a few common misunderstandings around cancer. Share this information with people as you gather this holiday season. It could ease others’ cancer fears.
Fortunately, this is incorrect. According to the National Cancer Institute Office of Cancer Survivorship, as of January 2022, it is estimated that there are 18.1 million cancer survivors in the United States. This represents approximately 5.4% of the population. The number of cancer survivors is projected to increase by 24.4%, to 22.5 million, by 2032.
Advances in the prevention, screening and treatment of cancer are improving cancer survivorship tremendously.
Generally speaking, no, cancer cannot be “caught” from another person. It is also true that certain cancer-causing viruses and bacteria passed from one person to another can increase the likelihood of developing cancer. In rare circumstances involving transplantation or pregnancy, transmission has been known to occur.
While some of us are born with genes passed down from our parents that may predispose us to developing cancer at some point in our lives, only about 5-10% of cancers are due to mutations inherited from a parent. Most cancers are caused by genetic changes that occur and build up from lifestyle choices and/or exposure to chemicals and environmental factors during our lifetime.
Everything around us causes cancer.
Who hasn’t heard that using deodorant, cosmetics, hair dyes, smart phones, microwaves, sugar, artificial sweeteners, or being in close proximity to power lines all can cause cancer?
The good news: there is no consistent, conclusive scientific evidence to support these claims.
When you hear new or suspicious information about cancer, it’s a good idea to fact check by discussing it with your doctor. If you prefer to do your own online research, visit reliable cancer organization websites like these to find credible information you can trust. And, of course, there is a wealth of information on Bag It Cancer’s Resource Center.
National Cancer Institute
American Society of Clinical Oncology (ASCO)

by Bag It Team | Nov 8, 2022 | Educational Articles
For many people, having a trusted friend or family member join them during a doctor’s visit or test (in person, virtually, or by phone) can be a great source of comfort and practical help. Sitting in may also bring you some peace of mind.

Besides being there for support and a second set of eyes and ears, you may also be that person’s advocate—gathering and sharing information with the healthcare provider, collecting information for them, and following up after the appointment to ensure continuity of their care. Knowing what to do before, during, and after a medical appointment can help safeguard the health and well-being of your loved one.
The Bag It Cancer’s Bag contains a nifty take-everywhere binder that was designed to help people get prepared for their medical appointments, keep track of information and records in an organized manner, and accompany them to each visit. Here are some of the tips from the binder.
Prepare for the appointment
- Set time aside with your family member or friend to discuss the primary purpose of the appointment. Is this a check-up? Follow up visit? Possible new medical condition? Together make a written list of questions, notes, or updates to share with the provider, keeping it to a single page and leaving room for the answers). This might include new symptoms, possible side effects of medications, or a new medical condition since the last visit. Also, discuss how they would like you to assist them during the appointment so you come to an agreement about your role.
- Star the three top priorities on your list to discuss in case you don’t get to all of them. Some people prefer to make an extra copy to hand directly to the doctor at the start of the visit.
- Gather everything needed for the appointment. Use Bag It’s My Companion Guidebook to store and record all your information in the tabbed sections and on the helpful patient forms. You will need:
- Day/date/time of the appointment. (Note that providers often ask you to arrive earlier to complete paperwork.)
- Name, address, phone number of the provider’s office.
- Driving directions if needed. If someone is attending virtually or by phone, make sure you have the log in or call-in details in advance.
- Insurance cards and copays due at the time of service.
- Copies of your medical records, including medical and family history.
- A notebook, pen or a recording device such as a smart phone with recording app.
- A complete and accurate list of current medications, vitamins/supplements, and over the counter medicines being taken.
- If lab work, tests, imaging, or other procedure needs to be completed so the doctor can review the results at your appointment, schedule them in advance and with enough time for the report to be available to the provider. Call to make sure the results have been received by the doctor’s office. Or pick up a copy of the results and bring it with you to your appointment, if needed.
- If communication with the provider will be difficult for the patient due to a language barrier, request that a professional interpreter be present during the appointment. Relying on a family member or friend to perform this role is not the best choice when complicated medical terms may be used to discuss the patient’s diagnosis and treatment options, or difficult treatment decisions may need to be made.
- If you decide to go online to research the patient’s disease or condition, avoid misinformation by visiting only reliable medical websites. Download our tips on how to evaluate medical websites. Always discuss with the provider any information you find online to make sure it is appropriate for your loved one and their situation.
The information and forms are just what is needed to assist with recording your cancer journey. The guidebook gives information to help explain and understand what to expect and record for the future. The bag helps you feel more comfortable speaking up for yourself by providing forms to write down questions and concerns which will help to explain at future doctor appointments.
–Caregiver, California
During the appointment
- Introduce yourself to the provider if you have not met them and explain your role and who you are to the patient. If you will be attending appointments on a regular basis, begin to build your relationship as a member of the patient’s care team.
- If your loved one is unable or hesitant to actively communicate with their provider, speak up on their behalf early in the conversation if this is what was agreed to by you and the patient.
- Verify the doctor has received the results of testing or procedures completed since the last visit. Provide a copy of the results if they have not been received.
- Address the priority concerns and questions on your list. Be direct, honest and respectfully assertive when speaking with the provider.
- Listen carefully. Take notes and write the down the answers to the questions asked. Another idea is to record the conversation, with the provider’s permission. There are apps to download onto a smartphone, or use another recording device.
- Before the visit concludes, make sure any information relayed to you is well understood, including how to perform any medical tasks required at home. If not, ask for it to be explained again in a different way or using everyday language. Ask follow-up questions as needed. Repeating or rephrasing the important parts back to the provider are good ways to confirm you interpreted the information correctly.
- You can also ask for information to be provided to you in writing so you can refer to it at home. This is especially helpful for instructions on how to perform home care tasks.
- Review the patient’s current medications. Understand why any new medications are being prescribed, and make sure you are clear on how, how much and when the medicine should be taken to avoid medication errors.
- Find out the best way to communicate if a non-urgent matter arises between visits. Some offices prefer a message sent through the portal, some use email, and some will ask you to call a specific member of the health care team. If your loved one agrees, consider giving the provider your phone number and/or email as another point of contact.
- If there wasn’t enough time to address all the questions and concerns with the doctor, ask if a nurse or other member of the healthcare team can help you further that day, or follow up with you after the visit. You can also ask to make another appointment to continue the conversation.
- Request copies of any test results, reports or other medical records related to the appointment if not given to you automatically. If they are available online through the patient portal, confirm you have the correct URL for the website and instructions on how to set up a user name and password.
- Before leaving the office make any follow up appointments needed, if possible. Be sure any orders for lab work or other testing or procedures are given to you or sent electronically to the medical facility. This also includes any referrals to other providers.
After the Appointment
- Recap the visit with your loved one. Finish writing any notes or instructions you didn’t jot down in the office. Listening to the recording of the visit would be helpful here.
- Update the patient’s file with any new reports, test results or other documents you received during the visit. Download and print a copy to file if they are online in the patient portal.
- Fill all prescriptions promptly. Verify the pharmacy has a complete and accurate list of all the patient’s medications to avoid drug interactions. Report to the doctor any new symptoms or side effects that could be related to new medicines the patient is taking.
- If any lab work, tests or procedures, or referrals to other doctors were ordered during the visit, schedule these appointments in a timely manner. Ask when and how you will receive the results. Be sure to follow up with the office if you do not receive the results within the expected time frame –do not assume “no news is good news.” If you do not understand the results, reach out to the provider’s office for an explanation of what they mean.
We hope that these tips guide both you and your loved one to better health and more peace of mind.

by Bag It Team | Oct 10, 2022 | Educational Articles
 October is Health Literacy Month. A study by Health & Human Services Office of the Surgeon General showed that only about 12% of Americans have proficient health literacy skills. Unfortunately, many adults lack good knowledge about their medical condition and treatment, and don’t know how to get information that is presented in a way they can understand. People report having difficulty completing medical forms and relaying important details to their doctor about their health. They may not be able to accurately read directions to take their medicines as prescribed. Each of these common situations can be linked to poor health outcomes.
October is Health Literacy Month. A study by Health & Human Services Office of the Surgeon General showed that only about 12% of Americans have proficient health literacy skills. Unfortunately, many adults lack good knowledge about their medical condition and treatment, and don’t know how to get information that is presented in a way they can understand. People report having difficulty completing medical forms and relaying important details to their doctor about their health. They may not be able to accurately read directions to take their medicines as prescribed. Each of these common situations can be linked to poor health outcomes.
Bag It Cancer is committed to expanding health literacy for all populations. Our Bag It Bag is all about making sure that anyone with cancer can find, understand and use reliable information to make decisions about their health and guide them through a complex cancer care system.
For nearly 20 years we have worked with healthcare providers who make it a practice to give Bag It Bags to their patients at diagnosis. Having a bag of printed, clear, easy to understand materials from trustworthy cancer organizations, with customizable tools to make it their own, helps people get involved in their care and feel a bit more in control.
Let’s Start with The Basics in The Bag
- My Healthcare Team. Knowing who is on your healthcare team and what their role is points you in the right direction for your questions or other assistance.
- Cancer Words. There’s a short list of definitions for common cancer words, including cancer treatments, that you may not be familiar with but need to know.
- Lists of Questions to Ask. Asking the right questions at the right time helps you to get the info you need about your care and other areas of your life affected by a cancer diagnosis.
- Making Treatment Decisions. The bag walks you through what to consider as you make decisions about your treatment and care, including sources for more information about your cancer type and life situations.
- There’s a Lot to Keep Track of…medical records, appointments, business cards, questions and notes for the doctor, and lots and lots of paperwork. My Companion Guidebook has places for everything plus checklists to simplify the steps.
- Easy Tips and Hacks to Use Like these:
- If you’re not sure you understand what is being said to you by your healthcare team, ask for it to be explained again in everyday language (and in your preferred language). Then repeat the information back to the person to make sure you got it right.
- Bring someone to your appointments to listen and write down the information, or ask permission to record the visit. This will help to ensure accuracy and saves you from trying to remember everything that is said to you. Another idea is to ask for the information to be given to you in writing (and in your preferred language) so you can read it again at home.
by Bag It Team | Aug 31, 2022 | Educational Articles
September 20 is Take a Loved One to the Doctor Day. It’s a day set aside to remind us that some of our loved ones may need a little help when it comes to seeing a healthcare provider. Many people skip regular check-ups or wait until there is an emergency to visit a doctor. This could put them at risk for serious health issues.
There can be many issues holding someone back from a visit to the doctor’s office. Fear of doctors, needles, or tests. Access or not having a general practitioner they know. Concern about insurance coverage or other costs. Not having the time or not being in the habit of regular check-ups. Whatever is holding them back, having some extra support and encouragement could help them to schedule a much-needed visit.
When starting the conversation make sure to ask your loved one about their current health needs and write down any concerns they have regarding a visit. It can be a delicate conversation but here are some resources to help guide you.
“Most people don’t bring up the idea of going to the doctor in regular conversation. Days like Take a Loved One to the Doctor offer the opportunity to have those discussions with someone who might be resistant to get a routine check-up.”
—Dr. Rupesh Parikh, Comprehensive Cancer Centers’ Practice President
Resources To Help Your Loved One
This AARP guide provides advice regarding how to talk to your loved one about going to the doctor, being prepared for your appointment and other useful resources. They recommend that “you might need to turn on your powers of persuasion to get your loved one to agree to see a doctor. Many people have a long list of reasons for avoiding doctors’ visits. Don’t fight every point.”
The Comprehensive Cancer Center recommends teamwork, incentives and setting up the appointment once they agree.
Once the appointment is made, the American Cancer Society has some great tips for before, during and after the visit.
The Bag It Guidebook includes forms for medications, insurance contacts, medical information, list of questions, and an appointment summary log to help you prepare for, interact during and summarize the appointments. If you don’t have a Bag It bag, you can download the forms from our website.
“Most people don’t bring up the idea of going to the doctor in regular conversation,” said Dr. Rupesh Parikh, Comprehensive Cancer Centers’ practice president. “Days like Take a Loved One to the Doctor Day offer the opportunity to have those discussions with someone who might be resistant to get a routine check-up.”

by Bag It Team | Aug 9, 2022 | Educational Articles
In recognition of National Wellness Month, we wanted to look at how we can all take some simple, purposeful steps to be more active, manage stress, improve our mental and physical health and more. Not just for the month of August but all year long.
Whether you want to focus on physical, emotional, spiritual, or social wellness, it is important to pick one thing and get started with small steps that will help your new healthy habits stick around for the long term.
Build Wellness Into Your Life
Making a plan sounds daunting but wellness goals should be simple, easy to adopt and fit into your lifestyle.
Here are a few examples of what your wellness plan might look like:
- I want to focus on being active. I am going to start sitting less every day by setting an alarm to remind me to get up and walk for 1 minute every hour. Tip: Set that alarm in another room so you have to get up to turn it off.
- I want to focus on self-care. I am going to start by taking a 15-minute break, in a quiet location, with a book and my coffee/tea/favorite beverage on Monday, Wednesday and Friday. Tip: Create a favorite space (inside or outside) that is only used for taking a moment out of your day to decompress.

- I want to focus on managing stress. I am going to incorporate a 4-4-4 breathing exercise at 10 a.m. and 2 p.m. for 1 minute (breathe in for a count of 4, hold for a count of 4 and exhale for a count of 4). Tip: Practice this technique at any point in your day you might need to manage stress (driving, during a work meeting, while having a difficult conversation).
- I want to focus on physical and mental health. I am going to practice yoga for 20 minutes 3 times this week. Tip: purchase an online plan or sign up for a class (committing money helps us also commit the time).
- I want to focus on healthy eating. I will incorporate 1 fruit or vegetable into at least 2 meals every day this week. Tip: Focus on what is in season so it will be tastiest and also give you variety throughout the year.
Looking for a little inspiration to get started?
Here are some other ideas to put you on the road to a healthier, happier life:
- Increase your water intake. The Mayo Clinic tells us how much water is enough.
 Monitor your sleep and make adjustments for better sleep habits.
Monitor your sleep and make adjustments for better sleep habits.- Join a walking, or aerobics class.
- Learn to meditate. Mindful.org gives you some meditation tips. \Plan a day of fun activities you love.
- Visit with friends and family.
- Start a gratitude journal. PositivePsychology.com can get your started.
- Practice being your own cheerleader with positive self-talk.
Setting Goals That Stick
We’re talking about wellness goals that are easy to incorporate into your lifestyle. But if you want some help with setting a goal, here are a few steps you can take to create a wellness plan that will endure:
- Pick a topic you want to focus on.
- Set 1 goal using the S.M.A.R.T. method
- Specific: The goal should be very precise with no room for misinterpretation.
- Measurable: The goal should be quantifiable, and progress should be easy to track.
- Achievable: The goal should be attainable — not outlandish or unrealistic.
- Relevant: The goal should contribute to your broader, overarching goals.
- Time-bound: The goal should have a defined start and end date.
- Share your goal with a trusted friend or family member. Accountability can often help encourage our success. You also might find a goal buddy!
- Write it down and put it somewhere you can see it every day.
Other Resources
Defining Wellness
The Global Wellness Institute defines wellness as the active pursuit of activities, choices and lifestyles that lead to a state of holistic health. – Read more about the Global Wellness Institute’s perspectives.
Wellness at Work
Since we spend much of our waking hours at work, here is a WebMD Health Services’ article that shows how to promote employee wellbeing.
Stay tuned for our August podcast for more on the five dimensions of wellness.





 October is Health Literacy Month. A study by Health & Human Services Office of the Surgeon General showed that only about 12% of Americans have proficient health literacy skills. Unfortunately, many adults lack good knowledge about their medical condition and treatment, and don’t know how to get information that is presented in a way they can understand. People report having difficulty completing medical forms and relaying important details to their doctor about their health. They may not be able to accurately read directions to take their medicines as prescribed. Each of these common situations can be linked to poor health outcomes.
October is Health Literacy Month. A study by Health & Human Services Office of the Surgeon General showed that only about 12% of Americans have proficient health literacy skills. Unfortunately, many adults lack good knowledge about their medical condition and treatment, and don’t know how to get information that is presented in a way they can understand. People report having difficulty completing medical forms and relaying important details to their doctor about their health. They may not be able to accurately read directions to take their medicines as prescribed. Each of these common situations can be linked to poor health outcomes.



 Monitor your sleep and make adjustments for better sleep habits.
Monitor your sleep and make adjustments for better sleep habits.
Recent Comments