
by Bag It Team | Jul 3, 2024 | Educational Articles
Grilling is a fun and tasty way to cook, especially in the summer. But did you know there are ways to make your grilled food healthier? Here are some simple tips to keep your food yummy and safe:
- Pick Lean Meats: Choose meats with less fat like chicken breasts, fish, or lean beef. Fatty meats can cause flames to flare up and create harmful chemicals. Trim off any extra fat before grilling.
- Marinate Your Meat: Soak your meat in a tasty marinade before grilling. Marinades with vinegar, lemon juice, or herbs can make your food healthier and protect against harmful chemicals that form when meat is cooked at high temperatures.
- Grill More Veggies and Fruits: Grilled vegetables and fruits are delicious and super healthy. Try grilling bell peppers, zucchini, mushrooms, pineapples, or peaches. They don’t create harmful chemicals when grilled, and they taste great!
- Avoid Burning Your Food: Don’t let your food get too dark or burnt. Burnt food can have bad chemicals. Cook at a moderate temperature and flip your food often to avoid charring. If parts do get burnt, cut them off before eating.
- Keep Your Grill Clean: Clean your grill regularly to get rid of old grease and food bits. This helps prevent harmful chemicals from forming.
- Pre-Cook Your Meat: Cook your meat a little bit in the microwave or oven before grilling. This way, it doesn’t have to stay on the grill too long and you can avoid harmful chemicals.
By following these easy tips, you can enjoy delicious grilled meals that are healthier for you. Happy grilling!
by Bag It Team | Jun 3, 2024 | Educational Articles
In honor of National Cancer Survivors Day on Sunday, June 2nd, Bag It’s own Mikey Shock has shared her personal journey of coming to terms with being a cancer survivor.
Cancer Survivor… Survivorship… They are words that usually make one think of someone who has won the battle with cancer and is in remission. But there is so much more to survivorship than we think. Survivorship begins at the time of diagnosis and continues for the rest of your life, beyond treatment. It refers to the navigation and experience of a cancer diagnosis.
For the longest time during treatment, I felt like I couldn’t use the word survivor because I had not yet beat cancer; I wasn’t in remission yet. But, others told me that I was a cancer survivor. There was so much inner turmoil because how could I have cancer? I honestly thought it was REALLY funny that I had such a diagnosis. I grew up asking my Mom if I would get the cancer she had when I was two, and she would always tell me no because it isn’t genetic. Well… it’s funny because I got the same diagnosis in the same location, and during the same time of year, 19 years later.
 Cancer was one of the best and worst things that ever happened to me. I am so glad and grateful I had cancer. I learned so much about who I was and what I could do. Even though I know my diagnosis doesn’t define me, I now find myself constantly motivating myself by saying “I beat cancer, this is nothing!” Knowing that there is a possibility you could die because you have a deadly diagnosis changes your perspective on life and the world around you. You see things you never noticed before, you appreciate the world around you and the fresh air in your lungs (especially after you experienced a collapsed lung). My diagnosis changed me for the better.
Cancer was one of the best and worst things that ever happened to me. I am so glad and grateful I had cancer. I learned so much about who I was and what I could do. Even though I know my diagnosis doesn’t define me, I now find myself constantly motivating myself by saying “I beat cancer, this is nothing!” Knowing that there is a possibility you could die because you have a deadly diagnosis changes your perspective on life and the world around you. You see things you never noticed before, you appreciate the world around you and the fresh air in your lungs (especially after you experienced a collapsed lung). My diagnosis changed me for the better.
After months of coughing until I threw up and having my symptoms ignored by my doctor, I finally received a chest x-ray that showed my right lung collapsing and filling with fluid. Further scans at the ER revealed a massive tumor causing this destruction. After a hospital stay, lots of tests, and a month later I found out that it was Hodgkin’s Lymphoma. It was surreal because I grew up with my Mom sharing her experiences battling this diagnosis. I hear the horror she experienced because technology had not yet evolved to what it is today. I underwent 16 chemo treatments for ABVD and 15 rounds of radiation.
It wasn’t until after I was considered in remission that I started to truly process my survivorship. During treatment, I was in survival mode and wasn’t able to consider my feelings and emotions toward it, I had to get through it.
Ultimately what helped me process my survivorship was Bag It Cancer! I had read all of the materials in the binder during treatment, though I wasn’t able to process everything I was reading, I appreciated knowing I had a resource I could go to whenever I needed it. After I started working for Bag It, I began to see what a helpful resource the Bag It Bag could be. I started to attend events on behalf of Bag It where we would have an advocate table. One of my first events was a Survivorship event. I heard stories, participated in small groups, and had several discussions with oncologists and cancer survivors. This is when I started to truly process what I had just gone through!
After my treatments had ended, I became very depressed and I wasn’t sure why. I was honestly sad that I wasn’t in treatment anymore. I can’t explain it. It wasn’t survivor’s guilt, but a sadness that I had finished that journey. It also didn’t help that the cards, constant texts, and support were starting to dwindle because I was “fine” at that point. I just felt lost.
Honestly, coping with the experience of survivorship after treatment was way harder than during treatment. Again, I can’t tell you why, but I think it’s because I wasn’t in survival mode. I was finally given the time and energy to process this traumatic experience.
I also felt (and still sometimes feel) completely invalidated. I feel that when my body hurts, or when I am so tired that I can’t function, or that I get confused and foggy it’s not a valid excuse anymore because I’m not in treatment. Even a year after treatment ended, I still feel these symptoms at full force and feel like I am expected to be at my full capacity even though I can’t. For some, these long-term symptoms last months, years or even for the rest of your life after chemo.
Survivorship to me means that I am someone who has battled and beat cancer, but also continuing the battle for the rest of my life. I was poisoned with some nasty stuff, and I came out stronger. I am proud of my journey. I am a cancer survivor, and each moment is my gift. Stay strong!

by Bag It Team | May 7, 2024 | Educational Articles
May marks Women’s Health Month, a time to raise awareness about the unique health needs of women. The demands of work and family, among other barriers, can greatly affect many women’s abilities to take care of their own health. This month’s spotlight on women serves as a gentle reminder for them to prioritize their own physical, mental, and emotional well-being.
Consider the “whole” you, with these practical tips:
- Make good food and drink choices – avoid processed foods and sugar; focus on fruits, veggies, whole grains, lean protein
- Stay active – Exercise or do other physical activity you enjoy, and often
- Get preventive healthcare – have regular checkups and screenings recommended by your doctor
- Foster emotional well-being – cultivate resilience, practice self-care, nurture healthy relationships, and find balance in your daily life
Remember to “mind your mind” by tending to your mental health just as you would care for your physical health.
Research shows that maintaining a healthy lifestyle can help to lower your risk of many different health conditions, including cancer. Bag It Cancer recognizes the importance of having trustworthy resources specifically for women’s cancers. That’s why we collaborated with national women’s cancer nonprofits to create two Bag It Bags for metastatic breast and uterine cancers. Each bag has introductory information about these specific cancer types and the supportive resources offered by our partners. Order a Bag for yourself or a loved one.
Resources for Women’s Health
Know Your Rights: Reproductive Health Care from the Office on Women’s Health Women’s
Women’ Health from the Centers for Disease Control and Prevention (CDC)
National Institutes of Health (NIH) – Office of Research on Women’s Health
by Bag It Team | Apr 10, 2024 | Educational Articles
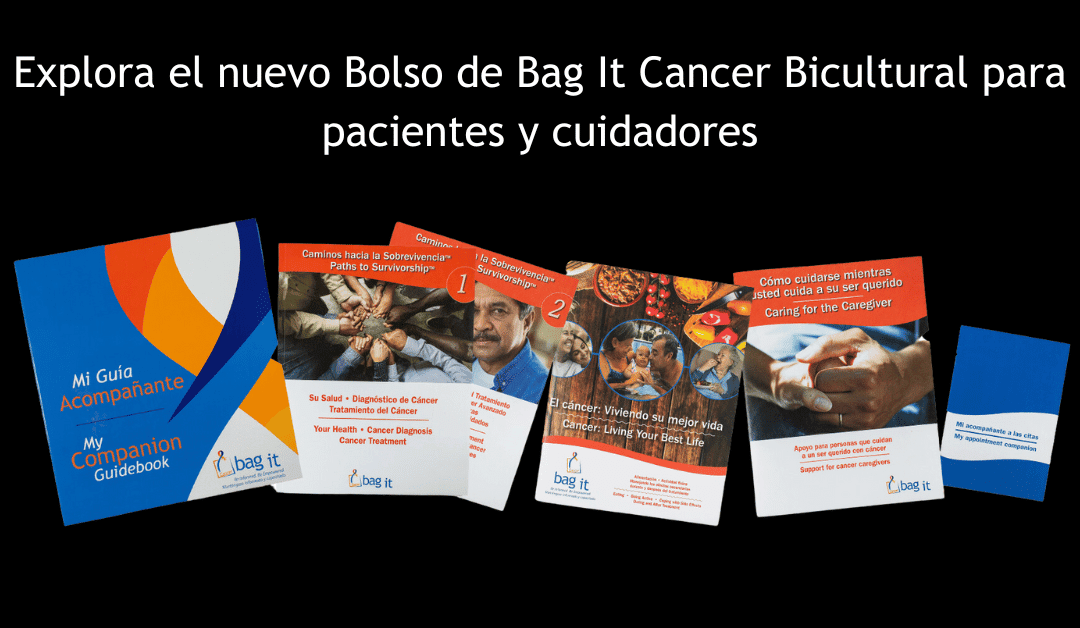
Diseñado específicamente para la comunidad Latina y sus familias que enfrentan cáncer, este Bolso es el resultado de dos décadas de experiencia y colaboración para mejorar el contenido del Bolso Bag It original en español.
 Reconociendo la profunda influencia de las creencias y los valores culturales durante el trayecto del cáncer, trabajamos estrechamente con miembros de la comunidad Latina que han tenido su propia experiencia con el cáncer: los sobrevivientes, los cuidadores, los proveedores de atención médica y otras personas que atienden a personas con cáncer. ¿El resultado? Un recurso único disponible tanto en español como en inglés, diseñado para cumplir con las necesidades de esta comunidad.
Reconociendo la profunda influencia de las creencias y los valores culturales durante el trayecto del cáncer, trabajamos estrechamente con miembros de la comunidad Latina que han tenido su propia experiencia con el cáncer: los sobrevivientes, los cuidadores, los proveedores de atención médica y otras personas que atienden a personas con cáncer. ¿El resultado? Un recurso único disponible tanto en español como en inglés, diseñado para cumplir con las necesidades de esta comunidad.
El Bolso Bicultural en Español le da prioridad a la participación familiar, reconociendo el importante papel que desempeñan las familias en las decisiones de tratamiento y cuidado. También se incluyen las necesidades de los niños, con orientación específica sobre cómo apoyarlos a través de una comunicación y comprensión apropiadas para su edad. Profundiza en cómo un diagnóstico de cáncer impacta la dinámica familiar, ofreciendo apoyo tanto a los pacientes como a quienes los rodean.
El Bolso Bag It sobresalta la importancia de mantener su atención médica preventiva y sus exámenes de detección del cáncer con regularidad. Analiza conceptos erróneos comunes sobre el cáncer, y al mismo tiempo proporciona información objetiva y confiable sobre los fundamentos del cáncer con el propósito de empoderar a las personas mientras navegan las aguas de su propia experiencia con el cáncer.
 La comunicación efectiva es clave, por lo que el Bolso ofrece consejos y estrategias prácticas para fomentar el diálogo entre familiares y profesionales de la salud, incluida la búsqueda de apoyo de parte de trabajadores sociales, asesores espirituales y otras personas a medida que los individuos y quienes los rodean hacen frente a la experiencia del cáncer desde su punto de diagnóstico hasta el final en cada fase de la sobrevivencia. Esto incluye la importancia de utilizar intérpretes médicos, cuando corresponda, para garantizar que las personas sean escuchadas y comprendan la información que se les comunique.
La comunicación efectiva es clave, por lo que el Bolso ofrece consejos y estrategias prácticas para fomentar el diálogo entre familiares y profesionales de la salud, incluida la búsqueda de apoyo de parte de trabajadores sociales, asesores espirituales y otras personas a medida que los individuos y quienes los rodean hacen frente a la experiencia del cáncer desde su punto de diagnóstico hasta el final en cada fase de la sobrevivencia. Esto incluye la importancia de utilizar intérpretes médicos, cuando corresponda, para garantizar que las personas sean escuchadas y comprendan la información que se les comunique.
El Bolso de Bag It Cancer Bicultural en español es un recurso integral lleno de contenido y herramientas valiosos para empoderar a las personas y familias que enfrentan el cáncer. Proporcionar herramientas de organización e información confiable ayuda a que los pacientes obtengan una mayor sensación de control en su trayecto. La participación proactiva en su atención permite una mejor calidad de vida y resultados de salud.

by Bag It Team | Apr 8, 2024 | Educational Articles
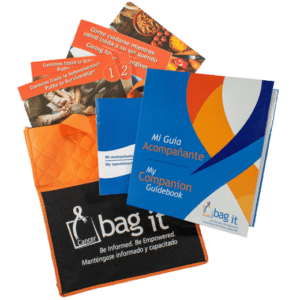
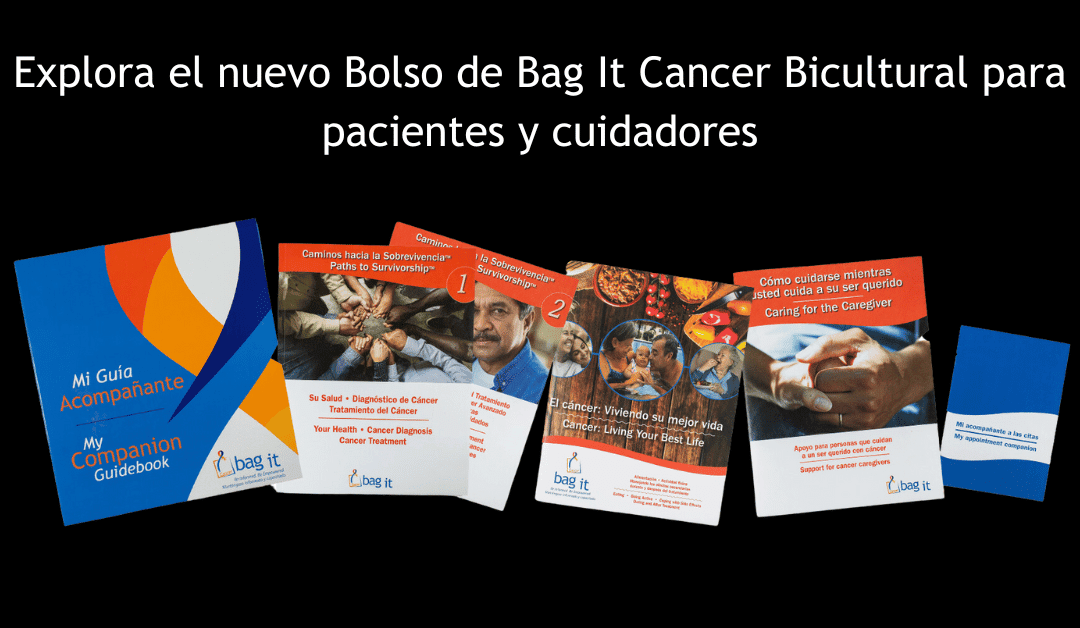
Crafted specifically for Latino and Hispanic individuals and their families facing cancer, this new Spanish Bicultural Bag It Bag is the result of two decades of experience and collaboration to enhance content in the original Spanish Bag It Bag.
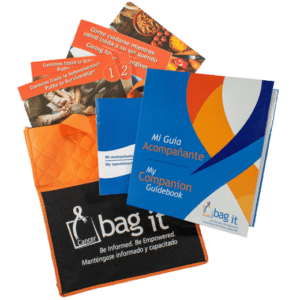 Recognizing the profound influence of cultural beliefs and values on the cancer journey, we worked closely with Latino and Hispanic individuals who have firsthand experience with cancer: survivors, caregivers, healthcare providers and others who serve people with cancer. The result? A unique resource available in both Spanish and English, tailored to meet the needs of these communities.
Recognizing the profound influence of cultural beliefs and values on the cancer journey, we worked closely with Latino and Hispanic individuals who have firsthand experience with cancer: survivors, caregivers, healthcare providers and others who serve people with cancer. The result? A unique resource available in both Spanish and English, tailored to meet the needs of these communities.
The Spanish Bicultural Bag prioritizes family involvement, acknowledging the significant role families play in treatment decisions and caregiving. Children’s needs are also addressed, with specific guidance on supporting them through age-appropriate communication and understanding. It delves into how a cancer diagnosis impacts family dynamics, offering support for both patients and those around them.
The Bag underscores the significance of maintaining regular, preventive healthcare and cancer screenings. It discusses common misconceptions about cancer while also providing reliable, factual information about cancer fundamentals to empower individuals as they navigate their unique cancer experience.
 Effective communication is key, so the Bag offers practical tips and strategies for fostering open dialogue among family members and healthcare professionals, including seeking support from social workers, spiritual advisors, and others as individuals and those around them navigate the cancer experience from diagnosis and through every phase of survivorship. This includes the importance of using medical interpreters, where applicable, to ensure individuals that their voices are heard, and they understand the information being relayed to them.
Effective communication is key, so the Bag offers practical tips and strategies for fostering open dialogue among family members and healthcare professionals, including seeking support from social workers, spiritual advisors, and others as individuals and those around them navigate the cancer experience from diagnosis and through every phase of survivorship. This includes the importance of using medical interpreters, where applicable, to ensure individuals that their voices are heard, and they understand the information being relayed to them.
Bag It Cancer’s Spanish Bicultural Bag is a comprehensive resource filled with valuable content and tools to empower individuals and families coping with cancer. Providing organizational tools and reliable information helps patients gain a greater sense of control over their journey. Proactive participation in their care allows for better quality of life and health outcomes.
Read more about this new Spanish Bicultural Bag in Spanish.
Read more about this new Spanish Bicultural Bag in English.
by Bag It Team | Feb 10, 2024 | Educational Articles
Many of us know that making healthy lifestyle choices and getting recommended vaccines can help lower the risk or EVEN prevent some kinds of cancer.
Cancer screenings, which are also cancer prevention strategies, check your body for cancer, even if you have no signs or symptoms. There are different kinds of screenings including:
- A physical exam and personal history
- Lab tests
- Imaging tests
- Genetic tests (these tests look for changes in the genes that may indicate that a person has or is at risk of having a particular disease or condition).
Routine screening tests can help to find breast, cervical, colorectal (colon), and other cancers early, when they may be easier to treat or cure. Many expert organizations provide guidelines for different screenings, but it’s important to talk with your doctor about your personal situation. There are benefits and risks for most screenings, and certain tests may be recommended only for people who are considered high risk for a particular cancer. Together you and your healthcare provider can decide which screenings are appropriate for you.
Remember! When your doctor recommends a screening test for you, it does not necessarily mean they believe you have cancer. Screening tests are used in people with average risk and no symptoms of cancer. Usually these tests, if abnormal, require additional testing to definitively diagnose cancer. If you have symptoms or increased risk based on your personal or family history, you may need to start screening at an earlier age than is typically recommended or may need specialized testing.
Questions to ask your doctor about cancer screenings
- Are any cancer screening tests recommended for me? Which ones?
- Can we talk about the test’s potential risks compared to its benefits?
- When should I start getting cancer screenings? And how often?
- What is the purpose of the test?
- What happens during the test?
- How long does it take to get test results?
- What happens if the results are not normal?
Screening & Prevention Resources
Centers for Disease Prevention & Control, How to Prevent Cancer or Find It Early: Screening
National Cancer Institute, Cancer Screening
Prevent Cancer Foundation, Cancer Screenings and Prevention
American Cancer Society, hundreds of articles on screening and prevention



 Cancer was one of the best and worst things that ever happened to me. I am so glad and grateful I had cancer. I learned so much about who I was and what I could do. Even though I know my diagnosis doesn’t define me, I now find myself constantly motivating myself by saying “I beat cancer, this is nothing!” Knowing that there is a possibility you could die because you have a deadly diagnosis changes your perspective on life and the world around you. You see things you never noticed before, you appreciate the world around you and the fresh air in your lungs (especially after you experienced a collapsed lung). My diagnosis changed me for the better.
Cancer was one of the best and worst things that ever happened to me. I am so glad and grateful I had cancer. I learned so much about who I was and what I could do. Even though I know my diagnosis doesn’t define me, I now find myself constantly motivating myself by saying “I beat cancer, this is nothing!” Knowing that there is a possibility you could die because you have a deadly diagnosis changes your perspective on life and the world around you. You see things you never noticed before, you appreciate the world around you and the fresh air in your lungs (especially after you experienced a collapsed lung). My diagnosis changed me for the better.
 Reconociendo la profunda influencia de las creencias y los valores culturales durante el trayecto del cáncer, trabajamos estrechamente con miembros de la comunidad Latina que han tenido su propia experiencia con el cáncer: los sobrevivientes, los cuidadores, los proveedores de atención médica y otras personas que atienden a personas con cáncer. ¿El resultado? Un recurso único disponible tanto en español como en inglés, diseñado para cumplir con las necesidades de esta comunidad.
Reconociendo la profunda influencia de las creencias y los valores culturales durante el trayecto del cáncer, trabajamos estrechamente con miembros de la comunidad Latina que han tenido su propia experiencia con el cáncer: los sobrevivientes, los cuidadores, los proveedores de atención médica y otras personas que atienden a personas con cáncer. ¿El resultado? Un recurso único disponible tanto en español como en inglés, diseñado para cumplir con las necesidades de esta comunidad. La comunicación efectiva es clave, por lo que el Bolso ofrece consejos y estrategias prácticas para fomentar el diálogo entre familiares y profesionales de la salud, incluida la búsqueda de apoyo de parte de trabajadores sociales, asesores espirituales y otras personas a medida que los individuos y quienes los rodean hacen frente a la experiencia del cáncer desde su punto de diagnóstico hasta el final en cada fase de la sobrevivencia. Esto incluye la importancia de utilizar intérpretes médicos, cuando corresponda, para garantizar que las personas sean escuchadas y comprendan la información que se les comunique.
La comunicación efectiva es clave, por lo que el Bolso ofrece consejos y estrategias prácticas para fomentar el diálogo entre familiares y profesionales de la salud, incluida la búsqueda de apoyo de parte de trabajadores sociales, asesores espirituales y otras personas a medida que los individuos y quienes los rodean hacen frente a la experiencia del cáncer desde su punto de diagnóstico hasta el final en cada fase de la sobrevivencia. Esto incluye la importancia de utilizar intérpretes médicos, cuando corresponda, para garantizar que las personas sean escuchadas y comprendan la información que se les comunique.
Recent Comments