by Bag It Team | Feb 9, 2026 | Educational Articles
 Cancer prevention can feel overwhelming — especially for individuals facing a diagnosis, caring for a loved one, or navigating survivorship. While not all cancers can be prevented, research shows that certain behaviors and informed decisions can help reduce risk and support long-term health.
Cancer prevention can feel overwhelming — especially for individuals facing a diagnosis, caring for a loved one, or navigating survivorship. While not all cancers can be prevented, research shows that certain behaviors and informed decisions can help reduce risk and support long-term health.
Prevention is not about blame or perfection. It’s about empowerment, access to accurate information, and progress over time.
At Bag It, we believe prevention, education, and support go hand in hand. By connecting people with trusted resources and practical tools, we aim to support informed decisions and healthier futures — and empower people to take small, meaningful steps.
What Does Cancer Prevention Mean?
Cancer prevention focuses on reducing risk where possible through lifestyle choices, early detection, and informed decision-making. These efforts not only support long-term health but can also help improve outcomes and quality of life.
 Actionable Ways to Support Cancer Prevention
Actionable Ways to Support Cancer Prevention
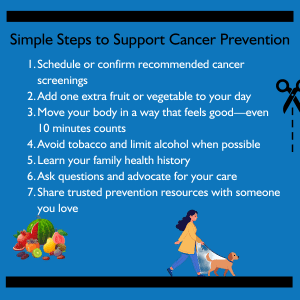
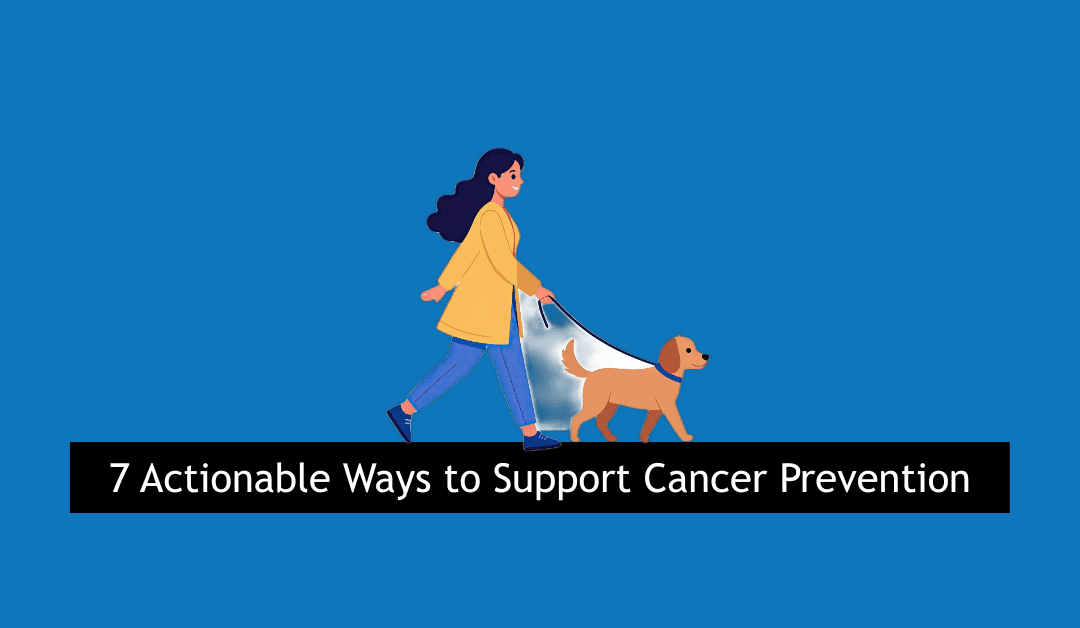
1. Stay Up to Date on Screenings
Regular screenings can help detect cancer earlier, when treatment may be more effective. Talk with a healthcare provider about screenings appropriate for your age, personal history, and risk factors.
2. Nourish Your Body
A balanced diet rich in fruits, vegetables, whole grains, and plant-forward foods supports overall health and may reduce cancer risk. Small changes — like adding one extra vegetable a day — can make a difference.
3. Move in Ways That Work for You
Physical activity doesn’t have to mean intense workouts. Walking, stretching, gardening, or gentle movement all count. Consistent movement supports physical and emotional well-being.
4. Avoid Tobacco & Limit Alcohol
Avoiding tobacco and limiting alcohol consumption are two of the most impactful steps individuals can take to reduce cancer risk.
5. Know Your Family History
Understanding your family’s health history can help guide conversations with healthcare providers and inform screening and prevention decisions.
6. Advocate for Yourself and Others
Ask questions, seek second opinions if needed, and encourage loved ones to stay informed. Prevention also includes access — to care, information, and support.
Prevention Is Part of the Bigger Picture
By sharing evidence-based resources and partnering with trusted organizations, we aim to meet people where they are — offering information that is practical, compassionate, and empowering across the cancer continuum.
Trusted Prevention Resources
We encourage exploring evidence-based resources from trusted organizations:
American Institute for Cancer Research (AICR)–Provides research-backed guidance on nutrition, physical activity, and lifestyle choices related to cancer prevention. AICR also contributes educational content included in Bag It bags.
American Cancer Society—Offers clear, accessible information on cancer prevention, screening guidelines, and healthy lifestyle choices.
National Cancer Institute (NCI)–NCI shares evidence-based cancer prevention and screening information for patients, caregivers, and providers.
Prevent Cancer Foundation—Focuses on prevention and early detection through education, awareness, and actionable screening resources.
And remember Bag It Cancer also consolidates information, tools and support from leading cancer organizations in our Cancer Resource Center.
by Bag It Team | Jan 13, 2026 | Educational Articles
Consider Health Goals That Meet You Where You Are
 January often brings messages about transformation—new habits, new routines, new expectations. For many people impacted by cancer, those messages can feel overwhelming or disconnected from reality.
January often brings messages about transformation—new habits, new routines, new expectations. For many people impacted by cancer, those messages can feel overwhelming or disconnected from reality.
Health doesn’t look the same for everyone, and it rarely follows a straight line. Treatment, recovery, caregiving, and survivorship all come with their own rhythms. Some days are about strength and momentum; others are about rest and simply getting through.
Rather than focusing on traditional resolutions, this season can be an opportunity to think differently about health—through smaller, more compassionate intentions. These intentions aren’t about fixing or improving yourself; they’re about noticing what you need and responding with care.
That might mean:
- Listening closely to your body and honoring rest without guilt
- Letting go of expectations about what health “should” look like
- Asking for support sooner, even when it feels uncomfortable
- Choosing movement, nourishment, or connection in ways that feel gentle and supportive
- Giving yourself permission to move at your own pace
For many people impacted by cancer, health goals are shaped by things outside of their control—treatment schedules, energy levels, emotions, and the needs of loved ones. In that reality, traditional goal-setting can feel unrealistic.
That’s why compassionate health goals begin with listening. Listening to your body, your emotional capacity, and what feels sustainable right now. These intentions allow for flexibility, rest without guilt, and adjustments when energy changes—while honoring mental and emotional well-being alongside physical health.
Health is not meant to be navigated alone. Support—from people, healthcare providers, and community organizations—plays an important role. At Bag It Cancer, our Bags are designed to be small reminders that care and connection can show up in simple, meaningful ways.
As the year unfolds, consider checking in with yourself often. Your needs may change, and that’s okay. Health intentions don’t need to be big or visible to matter. Sometimes the most meaningful steps are quiet ones, taken one day at a time.
Caring for yourself in ways that feel realistic and kind is always enough.
by Bag It Team | Dec 8, 2025 | Educational Articles
By Mindy Griffith, Executive Director
 As this year comes to a close, I find myself thinking about the many hands that have held a Bag It Bag, the conversations sparked by our resources, and the moments when someone realizes they are not facing cancer alone. Those stories stay with me. They remind me why this work matters—and how grateful I am for this community.
As this year comes to a close, I find myself thinking about the many hands that have held a Bag It Bag, the conversations sparked by our resources, and the moments when someone realizes they are not facing cancer alone. Those stories stay with me. They remind me why this work matters—and how grateful I am for this community.
In 2025, we reached more patients and caregivers than ever before, strengthened our relationships with healthcare providers, expanded our offerings with new cancer-specific bags to better meet the diverse needs of those navigating a diagnosis. Each step forward has been made possible because so many of you believe in the importance of empowering people with knowledge, support, and guidance during one of the hardest times in their lives. We truly couldn’t do this without you.
As you look ahead to the new year, we hope you’ll keep Bag It in mind. If someone in your life is facing a new cancer diagnosis—or if you want these resources for yourself—you can order a bag directly from us. And if you’re considering a year-end gift, your support helps ensure we can continue providing these tools to those who need them most. Monthly gifts, no matter the size, make a steady and meaningful impact all year long.
Thank you for being part of the Bag It community and for helping create moments of comfort, clarity, and hope. We look forward to all we can accomplish together in 2026.

by Bag It Team | Nov 10, 2025 | Educational Articles
By Kerri Reeves, LMSW, Oncology Support Services Manager, Oncology Social Worker , TMC Health Cancer Center
 Cancer. It’s a word that can shake the foundation of a person’s world—whether it’s your own diagnosis or that of someone you love. The emotional weight is immense, and the journey ahead can feel uncertain and overwhelming. But one of the most powerful ways we can help is simple: we show up.
Cancer. It’s a word that can shake the foundation of a person’s world—whether it’s your own diagnosis or that of someone you love. The emotional weight is immense, and the journey ahead can feel uncertain and overwhelming. But one of the most powerful ways we can help is simple: we show up.
Research by Evans Webb and colleagues (2021) highlights that cancer patients who receive consistent support from family and friends experience better emotional well-being, are more likely to follow treatment plans, and often have more favorable outcomes. Support matters. And showing up—physically, emotionally, and practically—can make all the difference.
Loved ones respond to a cancer diagnosis in many ways. Some are afraid—afraid of saying the wrong thing, afraid of the disease itself, afraid of the possibility of loss. That fear can lead to distance. Others may respond with overwhelming attention, reaching out constantly in ways that can feel smothering. And some may fade over time, as the initial shock wears off, and life pulls them in other directions.
So how do we support someone with cancer in a meaningful, balanced way?
We show up.
Showing up means being present. It means continuing to be part of their life—not just in the beginning, but throughout the journey. It can be as simple as offering to attend medical appointments and take notes, helping them remember what the doctor said. It might mean driving them to treatments or just sitting beside them in the waiting room.
 Showing up also means keeping life going. Talk to them about your day, share funny stories, laugh about your kids or grandkids—just like you always did. These moments of normalcy can be grounding and comforting.
Showing up also means keeping life going. Talk to them about your day, share funny stories, laugh about your kids or grandkids—just like you always did. These moments of normalcy can be grounding and comforting.
Practical help is another powerful form of support. Cook a meal. Organize a meal train. Help with chores like cleaning, taking out the trash, raking leaves, or walking the dog. These small acts of kindness can ease the burden and remind them they’re not alone.
And don’t stop showing up.
It’s okay to feel scared. It’s okay to feel overwhelmed. Supporting someone through cancer is emotionally taxing, and you may find yourself struggling too. If that happens, ask: who can show up for you?
Oncology social workers are trained to support not only patients but also their loved ones. You’re going through this too, and your feelings are valid. Whether you’re angry, in denial, sad, or even happy—it’s all part of the process. If you find yourself stuck in one of the darker places, it’s time to reach out for help.
Showing up is powerful. It’s healing. It’s human. And it’s something we can all do.
Here are some helpful resources that will guide you in your support journey.
- 16 Ways to Support Someone with Cancer
- Being a Friend to Someone with Cancer
- Appointment buddy or meal planner? 4 ways to support a friend with cancer
- How to Show Up When Your Friend Has Breast Cancer
Reference: Evans Webb, M., Murray, E., Younger, Z. W., Goodfellow, H., & Ross, J. (2021). The Supportive Care Needs of Cancer Patients: a Systematic Review. Journal of cancer education : the official journal of the American Association for Cancer Education, 36(5), 899–908. https://doi.org/10.1007/s13187-020-01941-9
by Bag It Team | Oct 8, 2025 | Educational Articles
By Ben Katsel, Associate Wealth Advisor at Mariner
A serious medical diagnosis can change life quickly—not just emotionally and physically but financially too. Amid new appointments, treatment plans and shifting priorities, it’s easy to push financial decisions aside. Yet creating a plan for times of change may help provide stability, clarity and peace of mind.
It’s helpful to understand the difference between financial advice and financial planning. Advice often focuses on answering specific questions, such as how to invest or where to save. Financial planning is broader: it’s an ongoing process of aligning your financial resources with your goals, values and needs. It considers your entire financial picture and is designed to help you make confident decisions, even when life feels uncertain.
Here are three foundational steps to help you begin:
Understand Your Current Financial Picture
Start by organizing what you have and what you owe. Review your income and expenses, including any new medical costs or changes to work. Identify your savings and emergency funds, ideally enough to cover several months of essential expenses, and list any debts and their terms. Finally, understand your insurance coverages—health, disability, and life—and how they might support you now.
This snapshot becomes the foundation for any future planning. It shows where you stand today and where adjustments may be needed.
Prioritize Flexibility Over Perfection
In uncertain times, financial plans should adapt. That might mean revisiting your budget to address new expenses or using tools like Health Savings Accounts (HSAs) or Flexible Spending Accounts (FSAs) for medical costs. Explore benefits such as short-term disability or Family and Medical Leave (FMLA) if income is affected.
The goal is progress, not perfection. A flexible plan that evolves with your situation is far more valuable than one that tries to predict everything in advance.
Balance Today’s Needs with Tomorrow’s Goals
Immediate concerns deserve focus, but small steps toward the future matter too. Consider reviewing beneficiary designations, updating estate documents and continuing to save for the long term, even if contributions are smaller for now. These actions are meant to help protect your future choices and keep your plan aligned with your goals.
Final Thought
Financial planning is a process designed to help create stability and confidence; it is not just about managing money. By taking small, intentional steps now, you can focus on building a plan that supports you and your loved ones through whatever comes next.
For additional guidance, the CFP Board’s overview of the financial planning process provides an excellent starting point. FINRA also provides helpful strategies for preparing for and navigating financial hardship, and the National Cancer Institute outlines track and manage cancer-related costs.
This article is for informational and educational purposes only and should not be construed as personalized advice. Financial planning cannot eliminate risk or uncertainty, and outcomes may vary based on individual circumstances. For additional information visit mariner.com.
by Bag It Team | Sep 5, 2025 | Educational Articles
 September 21 marks Take a Loved One to the Doctor Day—a national reminder that good health isn’t just a personal responsibility; it’s an important way we can support each other.
September 21 marks Take a Loved One to the Doctor Day—a national reminder that good health isn’t just a personal responsibility; it’s an important way we can support each other.
Whether it’s a parent, spouse, sibling, neighbor or friend, many people put off important medical appointments for reasons ranging from busy schedules to fear of bad news. But preventive care and regular checkups are essential for catching health issues early, managing ongoing conditions, and maintaining overall well-being.
Why This Day Matters
- Early Detection Saves Lives–Many serious health conditions, like cancer, diabetes, and heart disease, have better outcomes when detected early. More about early detection.
- Breaking Down Barriers–Some loved ones may face language, transportation, or cultural barriers to accessing healthcare. Your presence can help bridge those gaps.
- Emotional Support Counts–Going to a doctor’s appointment can feel intimidating. Having someone by your side can ease anxiety and encourage open conversations with healthcare providers.
 How You Can Participate
How You Can Participate
- Make an Appointment Together–Schedule a checkup for yourself and your loved one on or around September 21.
- Offer a Ride or Company–Even if you’re not the patient, being there for support can make a big difference.
- Help with Questions–Encourage your loved one to write down concerns or symptoms ahead of time so they get the answers they need.
- Celebrate the Step – After the appointment, enjoy a meal or activity together to mark the positive choice.
The Bottom Line
Good health is a gift we can help each other protect. This September 21 (or any day of the year), take the opportunity to show you care—by making sure someone you love gets the care they need. Sometimes, the best way to say “I love you” is with a ride to the doctor.
 Cancer prevention can feel overwhelming — especially for individuals facing a diagnosis, caring for a loved one, or navigating survivorship. While not all cancers can be prevented, research shows that certain behaviors and informed decisions can help reduce risk and support long-term health.
Cancer prevention can feel overwhelming — especially for individuals facing a diagnosis, caring for a loved one, or navigating survivorship. While not all cancers can be prevented, research shows that certain behaviors and informed decisions can help reduce risk and support long-term health.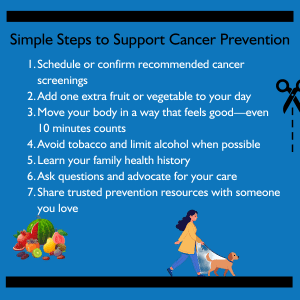 Actionable Ways to Support Cancer Prevention
Actionable Ways to Support Cancer Prevention
 January often brings messages about transformation—new habits, new routines, new expectations. For many people impacted by cancer, those messages can feel overwhelming or disconnected from reality.
January often brings messages about transformation—new habits, new routines, new expectations. For many people impacted by cancer, those messages can feel overwhelming or disconnected from reality.
 As this year comes to a close, I find myself thinking about the many hands that have held a Bag It Bag, the conversations sparked by our resources, and the moments when someone realizes they are not facing cancer alone. Those stories stay with me. They remind me why this work matters—and how grateful I am for this community.
As this year comes to a close, I find myself thinking about the many hands that have held a Bag It Bag, the conversations sparked by our resources, and the moments when someone realizes they are not facing cancer alone. Those stories stay with me. They remind me why this work matters—and how grateful I am for this community.
 Cancer. It’s a word that can shake the foundation of a person’s world—whether it’s your own diagnosis or that of someone you love. The emotional weight is immense, and the journey ahead can feel uncertain and overwhelming. But one of the most powerful ways we can help is simple: we show up.
Cancer. It’s a word that can shake the foundation of a person’s world—whether it’s your own diagnosis or that of someone you love. The emotional weight is immense, and the journey ahead can feel uncertain and overwhelming. But one of the most powerful ways we can help is simple: we show up. Showing up also means keeping life going. Talk to them about your day, share funny stories, laugh about your kids or grandkids—just like you always did. These moments of normalcy can be grounding and comforting.
Showing up also means keeping life going. Talk to them about your day, share funny stories, laugh about your kids or grandkids—just like you always did. These moments of normalcy can be grounding and comforting.
 September 21 marks Take a Loved One to the Doctor Day—a national reminder that good health isn’t just a personal responsibility; it’s an important way we can support each other.
September 21 marks Take a Loved One to the Doctor Day—a national reminder that good health isn’t just a personal responsibility; it’s an important way we can support each other. How You Can Participate
How You Can Participate
Recent Comments