by Bag It Team | Feb 8, 2022 | Educational Articles
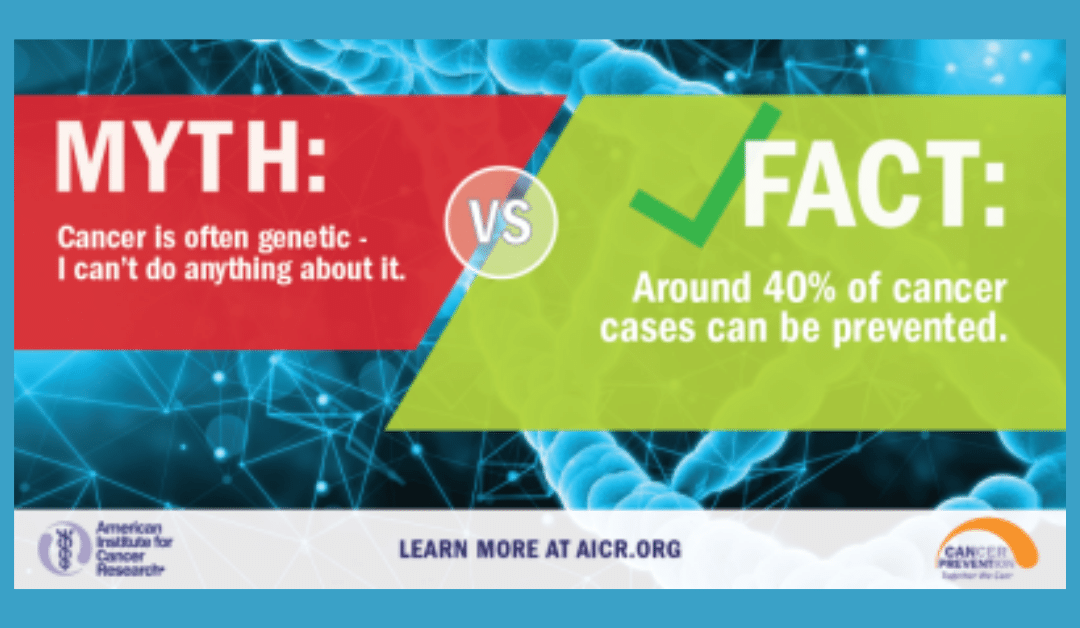
We wish we could say that all cancer is preventable if you just follow these steps, but that is not the case. However, research has shown that more than 40 percent of all cancers diagnosed can be attributed to preventable causes. That is why February is dedicated to cancer prevention.
Knowing the actions we need to take and actually taking them, does often require change in our lifestyle. Some of the actions we can take might feel a little easier such as not getting too much sun exposure, skipping the tanning bed, and making sure to have sun protection on when you are exposed. Some actions might feel more difficult like maintaining a healthy weight, quitting smoking, making different food choices and exercising regularly. A clean bill of health will show you the effort is worth it.

These behavior changes are listed as the top contributing factors for cancer prevention:
- Quit smoking: (this includes cigarettes, pipes, cigars, chewing tobacco and e-cigarettes) Tobacco use has been shown to increase the risk of developing 17 different types of cancer.
- Maintain a healthy weight: Being overweight or obese as an adult increases a person’s risk for 15 types of cancer. Talk to your doctor about what is a healthy weight for you.
- Be physically active: Being physically active reduces risk for nine types of cancer. Aim for at least 30 minutes of activity 5 times a week.
- Limit alcohol intake: Order smaller portions and drink a glass of water after every alcoholic beverage.
- Get regular screenings: American Cancer Society cancer screening guidelines by age.
- Get available vaccines: The Human papillomavirus (HPV) vaccine can significantly decrease the risk of several cancers including cervical, throat, tongue, anal, and other genital cancers. The Hepatitis B vaccine decreases the risk for liver cancer.
- Protect your skin from the sun: limit sun exposure between 10 a.m. and 4 p.m., make sure to wear sunscreen, clothing that covers your skin, and avoid tanning beds.
- Know your family history: Early detection can be key in life saving treatment. Knowing your family history can help you and your doctor plan for regular screenings (which may be recommended earlier with a known family history).
- Follow a healthy diet: AICR’s New American Plate, (⅔ whole grains, vegetables, fruit and beans, ⅓ protein), emphasizes foods that can reduce your risk for cancer and other chronic diseases.
There are lots of programs that can help you with weight maintenance, quitting smoking and alcohol intake. Talk to your doctor for any recommendations they feel might help. AICR’s website offers healthy recipes that contain cancer fighting foods.
If talking with your family about their health history feels difficult, practice with a friend first. Remind them that knowing their history can help you with early detection and prevention. If you do not have family available to ask about their history, talk to your doctor about genetic testing that may be available.
If getting started with activity is a little overwhelming or you don’t know what you like to do, many exercise programs have classes available online. If you find something you enjoy, you are much more likely to engage in activity regularly. Try lots of options and remember to start where you are.
In this month that focuses on LOVE, show yourself (and those who love you) some love by committing to lifestyle changes that will reduce your risk of being diagnosed with cancer. If you need a little extra support and accountability, you can take the pledge for AICR’s Click, Connect, and Commit campaign which offers a step-by-step guide to incorporate AICR’s 10 Cancer Prevention Recommendations in your everyday routine. You will also find a calendar with small steps you can take every day in February to help work towards your long term prevention goals.
by Bag It Team | Feb 1, 2022 | Podcasts
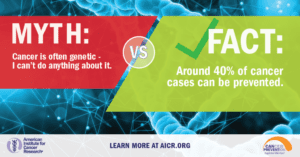
Did you know that 42% of cancers are potentially preventable? In this episode of Bag It’s podcast, Your Guide Through Cancer, host and Executive Director, Mindy Griffith chats with AICR’s Director of Nutrition Programs Sheena Patel Swanner. She provides simple lifestyle recommendations you can start today to help reduce your risk of cancer or a recurrence. Learn more and Take the Healthy 10 challenge today!

by Bag It Team | Jan 12, 2022 | Educational Articles
 Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).
Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).
Whether you personally have cancer or not, genetic testing can be helpful for your situation. If you have a cancer that was caused by a mutation, genetic testing can provide important information about how to treat your cancer, as well as your risk for developing a second cancer.
If you have not been diagnosed with cancer, genetic testing can estimate the likelihood of being diagnosed with certain types of cancer in your lifetime. The test can tell you if you have a higher risk than most people of developing those cancers, but not that you will definitely be diagnosed.
Most cancers are caused by acquired (somatic) variants which occur spontaneously during a person’s lifetime, often due to lifestyle and environmental factors. These variants are not passed on to the next generation. Sometimes, cancers can be common in a family but are not due to an inherited gene mutation.
If you do have a genetic mutation, you and your family members can take steps to manage your cancer risks and health care. Children of parents with an inherited cancer mutation have a 50 percent chance of having the mutation themselves.
Discuss your individual circumstances and family history of cancer with your doctor. Seek their advice on whether you should be referred for genetic testing, and which tests to have. Testing is a complex decision on multiple levels, with implications for your family as well. A genetic counselor is highly recommended before and after testing as interpreting the test results can also be complicated.
For more information about genetic testing, please visit these websites.

by Bag It Team | Jan 1, 2022 | Podcasts
Your Guide Through Cancer podcast host, Bag It Executive Director, Mindy Griffith interviews Stage 4 Cancer Survivor and Advocate Sheila McGlown. A wonderful example of what Bag It can do for you or your loved ones during this trying and worrying time. Join Mindy for this uplifting story.
Sheila uses her voice to raise awareness about the racial disparities faced by black women throughout their breast cancer journey. Receiving a breast cancer diagnosis is devastating for anyone, and Sheila passionately believes that racial disparities should not have an impact on the standard of treatment that black women receive.
by Bag It Team | Dec 1, 2021 | Podcasts
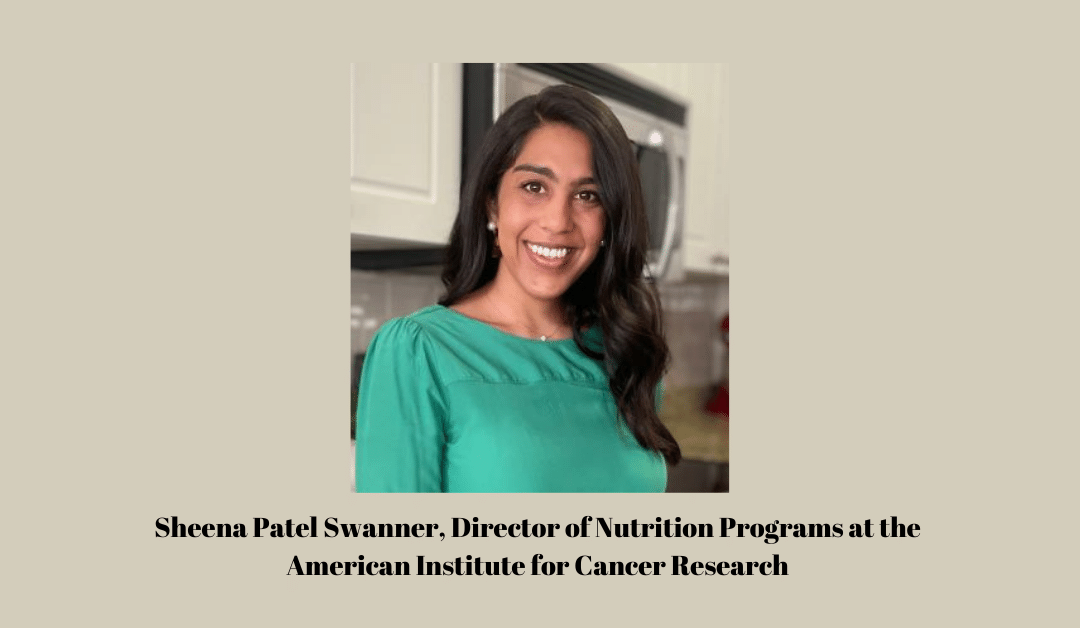
On this episode of Your Guide Through Cancer podcast, host and Bag It Executive Director, Mindy Griffith speaks with Dr. Rodgers Wilson, a forensic psychiatrist by training with an interest in transcultural psychology. They explore the effects of racial discriminations on health outcomes as well as the importance of early detection in cancer, sharing your personal history with your healthcare team and having the tools to move forward after a cancer diagnosis is critical to living your best life.
With over 30 years of clinical leadership experience, Dr. Wilson has worked with capitated provider organizations to improve population health management and instituted population health management strategies for health plans to impact the clinical care for high-risk clinical populations.
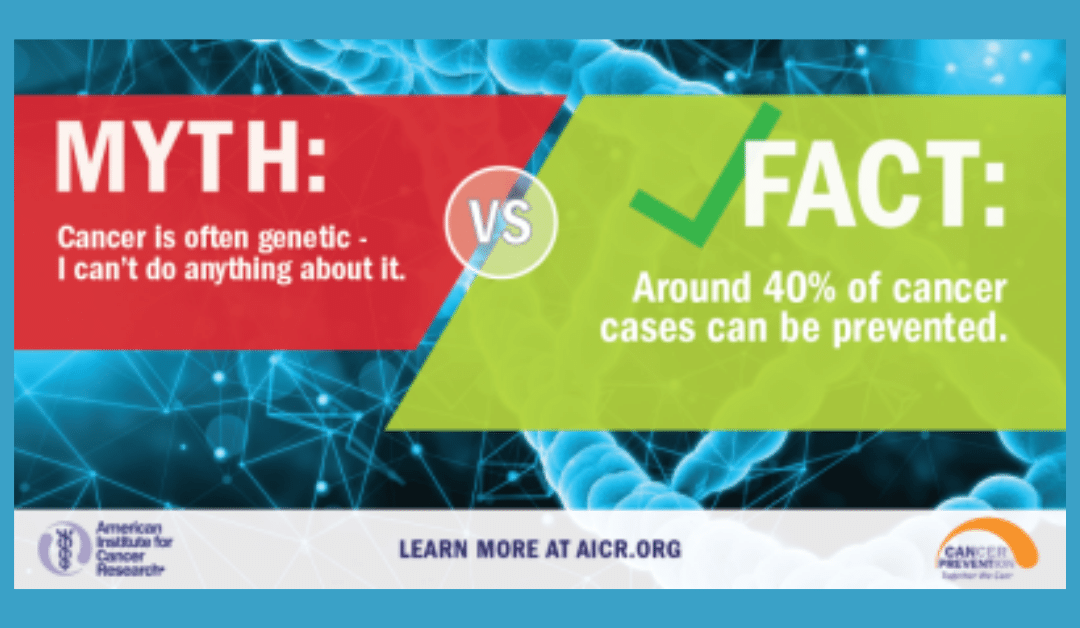






 Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).
Many people are shocked by their cancer diagnosis when no one in their family has been diagnosed with cancer. Cancer is caused by genetic changes (mutations or variants) in a person’s genes, chromosomes, or proteins, but that doesn’t generally mean it’s inherited from a parent. In fact, only about 5-10% of cancers are due to inherited cancer syndrome (germline mutation).

Recent Comments